FAQ: Donor high titre isohemagglutinin (anti-A/anti-B) testing at Canadian Blood Services
Authors: Melanie Bodnar, MD, FRCPC; Marc Bienz, MD, FRCPC; and Gwen Clarke, MD, FRCPC
Primary target audiences: Medical laboratory technologists (MLTs) in a hospital laboratory, transfusion medicine physicians
Background
Transfusion of ABO incompatible platelets or plasma can passively transfer isohemagglutinins (antibodies to red cell A and B antigens) to the recipient. These isohemagglutinins have the potential to cause hemolysis in recipients expressing the corresponding ABO antigens. The risk of hemolysis from ABO incompatible platelet and plasma transfusions can be minimized by selecting units that have been identified as having lower levels of isohemagglutinins.
As of November 2022, Canadian Blood Services has started performing automated isohemagglutinin titre testing (anti-A1 and anti-B) on all whole blood and apheresis donors. This testing will support the labelling of the following blood components as low titre: pooled and apheresis platelet concentrates and transfusable group A plasma. Implementation of the donor high titre assay and labelling of components as low titre will help support inventory management while mitigating the risk of acute hemolytic transfusion reactions (AHTR) during ABO incompatible platelet and plasma transfusion.
Frequently Asked Questions
1. How will donor high titre isohemagglutinin testing be performed?
All whole blood and apheresis donors will have automated anti-A1 and anti-B isohemagglutinin titre testing performed on each donation using the Beckman Coulter PK analyzer. Donor plasma diluted by the PK analyzer will be tested against A1 and B cells in separate wells at the same time as routine ABO and Rh typing on each donation. If both tests against A1 and B cells are negative according to the prespecified cut-off for the high titre assay, then the donor is considered to be a low-titre donor. Unlike testing performed in the hospital setting, high titre isohemagglutinin testing will be performed on the donor and NOT on the final component.
2. What titre cut-off will be used for determining which donors are low titre?
The titre cut off used by the PK analyzer is 1:32 which is equivalent to a dilution of approximately 1:128 at room temperature using the immediate spin manual method. A positive result on the PK analyzer would imply a manual titre to be ≥ to 1:128. To be considered low titre, the donor’s plasma must be negative at this dilution when tested against both A1 and B cells. All donors contributing to a platelet pool must test as negative on the PK analyzer in order for the component to be labeled as “Low Anti-A/B”. Donations that test as high titre using this assay are not excluded from use in transfusion, but the components manufactured from a high-titre donation are not labelled as low titre.
3. Why was a titre cut-off equivalent to 1:128 immediate spin selected for donor isohemagglutinin testing?
Acute hemolytic transfusion reactions due to the passive transfer of antibodies to group A and B red cells in ABO incompatible platelet transfusions are rare. Although there is not universal agreement on the testing method or titre cut-off value, the 1:128 manual titre was chosen based on the experiences of other blood suppliers and hemovigilance data, which appear to support its use as a safe cut-off value.
Automated methods using a cut-off value equivalent to 1:128 immediate spin have been adopted by other blood suppliers, including the Australian Red Cross Blood Service and the National Health Service Blood and Transplant (NHSBT) in the United Kingdom.1-3 While difficult to formally evaluate, the implementation of donor high titre testing in these countries appears to have reduced the risk of major adverse hemolytic events. Most AHTRs reported to surveillance systems have occurred at titres above this cut-off.
The optimal titre cut-off value must balance two considerations: (1) the safety imperative of identifying donors with the highest isohemagglutinin titres and (2) ensuring a reasonable proportion of components labelled as low titre will be available to benefit inventory management strategies.
Many hospital sites perform immediate spin isohemagglutinin testing on the final component at a lower threshold (such as 1:50). While immediate spin testing generally detects only IgM antibodies, validation studies indicate that automated testing using the PK analyzer can detect IgG isohemagglutinins, albeit not with the same degree of sensitivity as manual IAT (indirect antiglobulin phase) testing. This represents an important advantage of automated testing on the PK analyzer over manual immediate spin methods.
4. What are other advantages of using an automated method for isohemagglutinin titre testing?
Automated testing provides better efficiency, consistency and reproducibility compared to manual methods. Many facilities across Canada do not have the capability to perform isohemagglutinin titres. This large-scale testing at Canadian Blood Services ensures all facilities are able to provide components that lower the risk of AHTR when ABO incompatible platelets or plasma must be used.
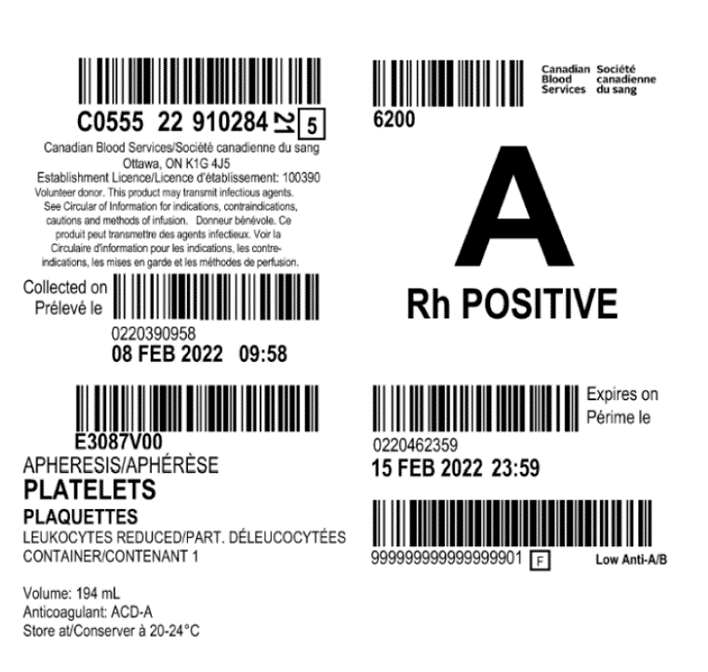
5. How will blood components be labelled to indicate that they are low titre?
Components that meet the low-titre criteria will be labelled “Low Anti-A/B” on the bottom right corner of the component label (see example of the label below). The same generic text will be used for all ABO blood groups. For blood group O, the donor must be negative for both high titre anti-A1 and anti-B isohemagglutinins to be considered low titre. As noted above, all donors in a pooled component, including both pooled platelets LR CPD (hereafter also referred to as untreated platelets) and pooled platelet psoralen-treated (hereafter also referred to as pathogen-reduced platelets) must test as low titre for the final component to be labelled low titre.
“Low Anti-A/B” will be both an eye-readable and bar-code readable attribute. Only low titre components will be labelled. Components that are unlabelled may be derived from one or more donors who did not meet criteria for being considered low titre or, less commonly, may not have been tested.
6. What blood components will be labelled as "Low Anti-A/B"?
The following blood components may be labelled as low titre:
- Group A, B and O pooled untreated platelets
- Group A, B and O pathogen-reduced platelets
- Group A, B and O apheresis platelets
- Group A plasma
7. Using this high titre assay, what proportion of donors are expected to test as low titre?
The proportion of donors that test as low titre will vary by blood group. Based on preliminary validation work, it is estimated that 60–70% of group O donors will test as low titre compared to 80–90% of group A donors and 85–95% of group B donors. It is expected that these numbers will be reflected in the relative proportion of apheresis platelets and transfusable group A plasma that are labelled as low titre. However, a significantly lower number of platelet pools will be labelled as low titre due to the requirement that all donors in a pool must individually test as low titre (see below).
There are many factors that can influence isohemagglutinin titre levels in a donor, including gender, age, recent infection or vaccination, and probiotic consumption. Canadian Blood Services will continue to gather data and refine estimates of the proportion of low titre donors by blood type.
8. If a pooled platelet concentrate is not labelled as “Low Anti-A/B”, is it still possible that the final component is low titre?
Yes. Untreated (i.e., not pathogen-reduced) pooled platelet concentrates require that all four donors in the pool must each individually test as low titre. If even one donor in the pool tests positive at the pre-specified cut-off value for either anti-A1 or anti-B, the final component cannot be labelled low titre, regardless of whether or not the plasma from the high-titre donor is used to create the pooled buffy coats. When four donors are combined in a platelet pool, the final component may still have a low titre even though it is not labelled as such. For more on how untreated pooled platelets are manufactured, see the Clinical Guide to Transfusion Chapter 2.
For pathogen-reduced platelets, the probability of labelling the final component as low titre with the current testing strategy will be further reduced as pathogen-reduced platelet pools are made using seven donors in a platelet pool. All seven donors must test low titre for the final pooled component to be labelled low titre. The optimal donor testing strategy for pathogen-reduced platelets is being investigated (see question 16).
9. Should hospitals that routinely perform high titre isohemagglutinin testing on platelet concentrates continue to do so?
Yes, although this will depend on an individual hospital’s needs. Hospitals that require more low titre-labelled platelet units than Canadian Blood Services is able to supply may continue to perform routine high titre isohemagglutinin testing on pooled platelet components. As noted in question 7, pooled platelet components may have low titres but do not have the low-titre label; hospitals can identify these low titre (but not labelled as low titre) units by testing the final blood component.
Based on donor testing results, it is estimated that 15–20% of untreated platelet pools will be labelled as low titre. By contrast, when the final pooled component is tested, up to 80% may test as low titre depending on the test method used. This difference in testing strategy (testing the donor versus testing the final pooled component) is addressed below. With implementation of high titre isohemagglutinin testing at Canadian Blood Services, more accurate data can be gathered regarding the relative availability of low titre labelled components.
10. Why is Canadian Blood Services performing high titre isohemagglutinin testing on donors and not on the final blood component?
Testing of components rather than donors would adversely impact manufacturing efficiency and may delay the distribution of platelet and plasma components. Testing of donors at the time of ABO and Rh testing can be performed efficiently and uses a process and automation strategy that has been effectively established by other blood suppliers.
11. How should low titre platelet inventory be distributed and used?
Depending on the availability of on-site isohemagglutinin testing capabilities, frequency of need for ABO incompatible platelet transfusion and local patient characteristics, each facility will need to determine how labelled low titre platelets can be optimally incorporated into existing inventory management strategies. For hospitals that use a hub and spoke model of distribution, preliminary modelling studies at Canadian Blood Services suggest that diverting labelled low titre platelet concentrates to smaller hospital sites that carry limited platelet inventory and that lack on site titration capabilities may help to reduce discard rates.4
12. How should low titre group A plasma inventory be distributed and used?
For hospital customers who currently have a policy to use group A transfusable plasma as emergency-release universal plasma (for example in the setting of trauma or massive hemorrhage protocols where the patient’s blood group is unknown), group A plasma tested and labelled as low titer may be a safer alternative because it further mitigates the risk for AHTR. Preliminary validation work estimates that 80–90% of group A donors will test as low titre. Hospitals may want to internally prioritize labelled low titre group A plasma inventory for use in this setting.
13. Can low titre blood components be specifically requested or ordered?
No. At this point, hospitals will NOT be able to specifically order low titre platelets or group A plasma. Platelet pools, apheresis platelets and group A plasma will continue to be distributed on a “first-in-first-out” basis to help maintain national inventory and avoid component wastage. The availability of low titre group A plasma is unlikely to be constrained given its long shelf life and the expectation that a relatively greater proportion of group A plasma will be labelled low titre. By contrast, it is estimated that only 15–20% of untreated platelet pools will be labelled as low titre and it is possible that this number will vary over time.
Ongoing surveillance of demand and availability may inform possible future changes to ordering practices.
14. Does donor isohemagglutinin titre testing eliminate the risk of acute hemolytic transfusion reactions due to ABO incompatible platelet or plasma transfusions?
Donor high titre isohemagglutinin testing is a risk mitigation strategy. The optimal platelet or plasma component for transfusion is one that is ABO identical, but when ABO incompatible platelets or plasma components must be used, a component that is labelled as low titre is safer than one that is untested or not labelled.
Recipients with a small blood volume (recipients of intrauterine, neonatal or pediatric transfusion) and those receiving a large cumulative volume of incompatible plasma infused over time may be at increased risk for a hemolytic complication despite the use of components labelled as low titre. This risk is further magnified when using apheresis platelet components (for
example, HLA and HPA selected apheresis platelets) that contain ABO incompatible plasma from a single donor. Other recipient factors and biologic characteristics of antibodies (aside from relative titre strength) may also influence the risk of acute hemolytic adverse events.
If an AHTR due to the use of components labelled as “Low Anti-A/B” is suspected, this should be reported to Canadian Blood Services following local procedures for reporting an adverse transfusion event (see our Guide to reporting adverse transfusion reactions).
15. Given that platelet inventory will include a mix of components across ABO blood groups both with and without low isohemagglutinin titres, how should a platelet unit be selected for transfusion to an individual patient?
Platelet concentrates from donors of the same ABO group as the patient are the optimal choice for transfusion.
While platelet recovery may be reduced in ABO incompatible platelet transfusions (i.e., recipient plasma contains isohemagglutinins against A and/or B antigens expressed on the platelet surface), this is usually not clinically significant. The most important consideration with respect to ABO incompatibility in platelet components is the presence of passively transferred donor isohemagglutinins that may be ABO incompatible with the recipient’s red cells, potentially causing an AHTR.
As noted above, this risk is highest in small pediatric/neonatal recipients receiving apheresis platelet concentrates which may contain a large volume of ABO incompatible plasma from a single donor and in recipients receiving cumulative ABO incompatible platelet transfusions.
Using group A platelets for group B patients (and vice versa) is preferred over group O if ABO identical components are not available.
In practical terms, the selection of the optimal platelet component for any given patient will depend on the inventory at hand. The following guide (Table 1) may be used to support decision making.
Table 1: Selecting the optimal platelet component for transfusion by blood group and low isohemagglutinin titre
| Recipient group | 1st choice | 2nd choice | 3rd choice | 4th choice | 5th choice |
|---|---|---|---|---|---|
| A | A | AB* | B (low titre) | O (low titre) | B>O |
| B | B | AB* | A (low titre) | O (low titre) | A>O |
| AB | AB | A (low titre) | B (low titre) | O (low titre) | A>B>O |
| O | O | B | A | AB* | / |
|
*Group AB platelets (very limited supply) should be prioritized for pediatric use. Caution is required when using low titre ABO incompatible platelets for IUT, pediatric, and neonatal recipients and recipients of all ages who are receiving multiple sequential ABO incompatible platelet transfusions. |
|||||
16. How will the implementation of pathogen-reduced pooled platelets at Canadian Blood Services impact isohemagglutinin levels in the final component and will isohemagglutinin testing still be necessary?
For pathogen-reduced pooled platelets, each donor contributing to the 7 donor pool must demonstrate low titer isohemagglutinins in order for the final product to be considered low titre. Platelet additive solution (PAS) is an integral part of the new manufacturing process for pathogen-reduced platelets at Canadian Blood Services. The use of PAS will reduce the isohemagglutinin levels in the final product due to the removal of approximately 60% of the plasma.5 However, preliminary reports from other blood suppliers suggests that donor high titre testing may still be warranted. Work is ongoing to determine the optimal donor isohemagglutinin testing strategy for pathogen-reduced platelets. For more about the manufacturing process for pathogen-reduced platelets, see our Clinical Guide to Transfusion Chapter 19, including the FAQ: Information for health professionals on pathogen-reduced platelets.
Additional resources
(Slide deck) Donor high titre isohemagglutinin (anti-A/anti-B) testing at Canadian Blood Services
References
- National Blood Service. Guidelines for the blood transfusion services in the United Kingdom, (The Stationary Office, 2013).
- Massey, E. High titre anti-A/B testing of donors within NHS Blood and Transplant (NHSBT). in Information documment INF178/4 (NHS Blood and Transplant, 2019).
- Cardigan, R., New, H.V., Estcourt, L., et al. International Forum on Policies and Practice for Transfusion of ABO and RhD Non-Identical Platelets: Responses. Vox sanguinis 117, e1-e20 (2022).
- Blake J, Clarke G., Bodnar M. Evaluating the Inventory Impact of Utilizing Low Titer Platelets in Regional Hospitals. Abstract presented at: The AABB Annual Meeting, 2022; Transfusion 62(S2), P-IV-7, 160A.
- Tynuv, M. & Flegel, W.A. Quality improvement with platelet additive solution for safer out-of-group platelet transfusions. Immunohematology 35, 108-115 (2019).