Blood: the basics
Authors: Sophie Chargé, PhD, and Kendra Hodgkinson, PhD
Online publication date: January 2017
What is blood?
With every heartbeat, about five litres of blood are pumped through your body.
Blood flows through thousands of kilometres of blood vessels, delivering oxygen and nutrients to the organs and carrying waste products away. Blood also transports cells, hormones and proteins that regulate many body functions, such as fighting infection and controlling blood loss.
What are the components of blood?
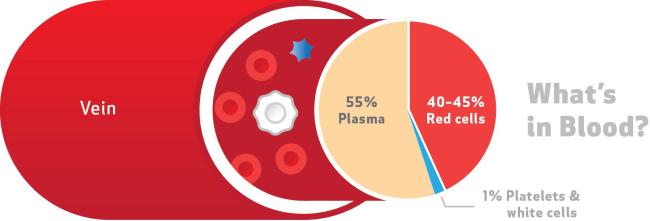
Blood is composed of four components: red blood cells, white blood cells, platelets, and plasma.
Red blood cells

- Red blood cells look like tiny doughnuts without holes; their red colour comes from hemoglobin, which is an iron-containing protein that binds to oxygen and carbon dioxide.
- Red blood cells use their hemoglobin to carry oxygen from the lungs to the tissues and organs. Red blood cells then pick up carbon dioxide from the tissues and organs and carry it back to the lungs for removal.
- In a healthy individual, a red blood cell stays alive for about 120 days. The average adult has about 25 trillion red blood cells. To maintain this level, the bone marrow in a person’s body produces 7.5 billion red blood cells every hour, or about 2 million a second.
- In transfusion medicine, red blood cells are isolated from donated whole blood and reconstituted in an additive solution that allows their storage at 4°C for several weeks (42 days for red blood cell units produced by Canadian Blood Services) until a patient requires a transfusion.
- When red blood cells are damaged (lysed) and their content is released into the blood, we say the blood is hemolysed. Red blood cells that are damaged can no longer carry oxygen and the released cellular content is toxic to the body. High levels of hemoglobin and other cellular debris can damage the kidneys.
White blood cells

- White blood cells help fight infections. When viruses or bacteria enter the blood, for example through a cut, a scraped knee or an infected ear, white blood cells surround and destroy the invading microorganisms (bacteria and viruses). The three main types of white blood cells are granulocytes, lymphocytes and monocytes.
- Granulocytes are the most abundant white blood cell and act as the first line of defense by “swallowing” microorganisms (phagocytosis) and killing them with enzymes stored in granules inside the cells.
- Lymphocytes recognize antigens on the surface of invading bacteria or viruses as “non-self”, then produce antibodies that disable the invading germs and target them for destruction.
- Monocytes support the activity of other white blood cells through phagocytosis and identifying targets to be destroyed by antibodies.
- Most white blood cells live for a few hours or days in the blood, so the bone marrow is constantly producing more. However, a small number of lymphocytes (sometimes called memory cells) live for many years to “remember” certain viruses and help the body resist being infected again. Vaccines work by triggering the body to produce these memory cells without actually making us sick.
- In transfusion medicine, white blood cells are removed from the final blood products. This procedure provides several benefits to patients receiving transfusions. Firstly, they are less likely to have a fever after their transfusion. They are also less likely to make antibodies against transfused donor cells, and so future platelet transfusion will remain effective. White blood cells may also harbour infectious disease agents such as cytomegalovirus (CMV). By removing them we reduce the risk of infection.
Platelets

- Platelets are small, delicate, plate-shaped cell fragments that help stop bleeding by sticking together and forming a clot that seals a hole in a blood vessel.
- Clot formation is triggered by the platelets coming into contact with torn blood vessels. This activates the platelets.
- Activated platelets become “sticky” and change shape, extending long, thread-shaped structures that help them clump together. The activated platelets interact with clotting factors in the blood to form a stable clot made of platelets held together by a mesh of protein (fibrin).
- At the surface of a cut or scrape, this plug becomes a scab to keep germs out of the body.
- Platelets stay functional for about 10 days in a healthy adult. New platelets are formed by cells called megakaryocytes in the bone marrow; each megakaryocyte releases thousands of platelets into the blood.
- In transfusion medicine, platelets are isolated from donated whole blood and reconstituted in plasma or a platelet additive solution (PAS) for storage prior to transfusion. Platelets can also be collected from a donor using an apheresis machine that allows the selective collection of platelets. Platelet units must be stored at room temperature and can only be kept for a few days prior to transfusion.
Plasma

- Plasma is the straw-coloured liquid that makes up more than half of the blood’s volume.
- Plasma acts as a transportation system for everything in the blood. About 90 per cent of plasma is water and the other 10 per cent is made up of the various materials being transported by the plasma.
- Plasma brings nutrients like proteins, minerals, vitamins, sugars, and fats to all parts of the body and carries away waste products. Plasma also transports the red blood cells, which carry oxygen and carbon dioxide to and from our organs and tissues.
- The constant circulation of white blood cells and antibodies in the plasma allows them to go anywhere they are needed to fight invading germs; similarly, circulating platelets and clotting proteins will be activated wherever blood clots are needed.
- Proteins that circulate in the plasma include albumin, antibodies and clotting proteins. Albumin is the most abundant protein in the plasma, and helps maintain fluid balance in your body by keeping water inside the blood vessels. Antibodies make up more than one-third of the protein in the plasma. Clotting proteins in the plasma are required for platelets to form blood clots.
- In transfusion medicine, plasma is isolated from donated whole blood. Plasma can also be selectively collected from donors using an apheresis machine. Plasma products can be stored frozen for long periods of time (up to one year at Canadian Blood Services) until required for a transfusion.
- In transfusion medicine, proteins such as albumin, immunoglobulins and clotting factors are isolated from plasma using a fractionation process. Once fractionated those proteins can be stored freeze-dried (lyophilised) for long periods of time and be used to treat specific medical conditions.
What are blood groups?

Blood groups are genetic, like the colour of a person’s eyes. There are four major blood groups: A, B, AB and O. Blood groups are based on red blood cell antigens, which are proteins on the cell surface that are recognized by a person’s immune system. If an antigen is identified as “non-self” by the immune system, the cell is targeted for destruction by antibodies.
Group A has one type of antigen (A), Group B has a different type (B), Group AB has both A and B antigens, and Group O does not have either antigen. These blood groups are further divided by whether or not an antigen called the Rh factor is present on the person’s blood cells. If it is present, that person’s blood is Rh positive (+); if not, the blood is Rh negative (-). Combining Rh factor with the four major blood types results in eight different main blood types (for example, AB-). In addition, there are minor blood groups.
An individual of a certain blood type will develop antibodies against the antigens that they don’t have. For example, a Blood Group A individual has no B antigens on their red blood cells; therefore, this person’s white blood cells will make antibodies against the B antigen (anti-B) that will be present in their plasma.
In transfusion medicine, it is very important that patients receive red blood cells that are compatible with their blood type. It is also important that plasma recipients are not transfused with plasma that contains antibodies that will destroy their red blood cells.
Blood types can be determined quickly by mixing a few drops of someone’s blood with anti-A, anti-B or anti-Rh antibodies and seeing which antibodies make the red blood cells clump together. This clumping happens when the antibodies match the antigens present on the red blood cells; for example, if someone’s blood clumps with anti-A but not with anti-B antibodies, this shows that the blood has A (but not B) antigens, making that person type A. In transfusion medicine, sophisticated assays are used to appropriately type the blood of the donor and of the patient.
What is meant by a blood match?
In the context of blood transfusions, a blood match is a compatibility between the donor’s blood and the recipient’s blood. This does not always mean an identical blood match.
Red blood cells from a donor that is type O+ can be transfused into patients of four different blood types: A+, B+, AB+, and of course O+. People with type O- blood are called universal donors because their donated red blood cells have no A, B or Rh antigens and can therefore be safely given to people of any blood group. People with type AB+ blood are universal recipients because they have no antibodies to A, B or Rh in their blood and can receive red blood cells from a donor of any blood type.
Plasma transfusions are matched to avoid A and B antibodies in the transfused plasma that will attack the recipient’s red blood cells. People with type AB blood are universal plasma donors. Their plasma does not contain A or B antibodies and can be transfused safely to all blood types.
Table 1. Blood type and compatibility.
| Blood type | Percent of Canadians | Blood types of compatible recipients (red blood cells) | Blood types of compatible recipients (plasma) |
|---|---|---|---|
| O- | 7 | All blood types | O-, O+ |
| O+ | 39 | O+, A+, B+, AB+ | O-, O+ |
| A- | 6 | A-, A+, AB-, AB+ | O-, O+, A-, A+ |
| A+ |
36 |
A+, AB+ | O-, O+, A-, A+ |
| B- | 1 | B-, B+, AB-, AB+ | O-, O+, B-, B+ |
| B+ | 8 | B+, AB+ | O-, O+, B-, B+ |
| AB- | <1 | AB-, AB+ | All blood types |
| AB+ | 3 | AB+ | All blood types |
Acknowledgements
This information is adapted from content developed by Canadian Blood Services for the Learning to Save Lives program. This program supports educators who are teaching concepts related to blood, stem cells, and tissue and organ donations.