Chapter 4
Immunoglobulin products
Background
Immunoglobulin (Ig) products are manufactured from plasma collected from a large number of carefully screened donors. Ig products may be used as replacement therapy for immunodeficient patients or as immunomodulatory therapy for autoimmune and alloimmune disorders. Ig products include intravenous Ig (IVIg), subcutaneous Ig (SCIg), and hyperimmune globulins such as RhD Ig (RhIg).
Patients receiving Ig products may have reduced response to immunization with parenteral live virus vaccines but IVIg has minimal interference or interaction with inactivated viruses, live oral vaccines, live intranasal vaccines and the Bacillus Calmette–Guérin (BCG) vaccine. For guidance, please refer to the Canadian Immunization Guide from the Public Health Agency of Canada.1
Immunoglobulin products
Immunoglobulin products are sterile solutions or lyophilized concentrates of human immunoglobulin G (IgG) that have been processed to remove multimers and aggregates of IgG, allowing intravenous infusion. The distribution of IgG subclasses in Ig products is similar to the human plasma. Depending on the method of preparation, some commercial products may contain trace amounts of other immunoglobulin classes: IgA, IgM, IgE and IgD.
The various products differ in their manufacturing processes, in terms of plasma pool sizes, steps to improve Ig yields, removal of contaminants, pathogen inactivation technology, and use of stabilizing or preservative agents. The relevance of such modifications has not been established and different products may be used interchangeably in clinical practice.2,3
After infusion of Ig, the various passively transferred antibodies in the patient’s blood may yield positive serological testing results, with the potential for misleading interpretation. Passive transmission of antibodies to red cell antigens (e.g., A, B, and D) may cause a positive direct or indirect antiglobulin (Coombs) test. For this reason, serological testing results for other antibody-mediated tests (e.g., hepatitis B core antibody [anti-HBc], hepatitis A, varicella) may also be misleading. Because of this, consideration should be given to performing hepatitis B testing with hepatitis B surface antigen (HBsAg) in patients before Ig therapy is initiated to inform the risk of hepatitis B reactivation.4,5
For the names and product-specific details of the Ig products carried by Canadian Blood Services, see Canadian Blood Services’ national e-formulary for plasma protein and related products. Please refer to the manufacturer’s product monograph for the most up-to-date information on indications, dosing, administration and potential side effects.
Intravenous immunoglobulin
Mechanism of action
Although the mechanism of action for IVIg has not yet been clearly elucidated, the proposed mechanisms are described in Table 1.
Table 1: Proven and hypothesized mechanisms of action of IVIg with some evidence6-8
| Use | Mechanism of action | References |
|---|---|---|
| Protection against infection and supplementation for congenital/primary and acquired/secondary immune deficiency |
|
9, 10 |
| Immune modulation in autoimmune or modulatory conditions |
|
6, 8, 11, 12 |
| Prevention of alloimmunization against RhD with RhIg |
|
13-15 |
Indications
The licensed indications for IVIg in Canada vary slightly by product but currently include:
- Primary immune deficiency (PID)
- Immune thrombocytopenic purpura (ITP)
- Secondary immune deficiency (SID) states
- Chronic inflammatory demyelinating polyneuropathy (CIDP)
- Guillain-Barré syndrome (GBS)
- Multifocal motor neuropathy (MMN)
IVIg is often used as an off-label therapy for diseases that may have an immune-mediated or unknown etiology. This off-label use accounts for a significant proportion of IVIg use in most Canadian provinces.16
In the attempt to ensure appropriate utilization of IVIg, many jurisdictions across Canada have developed policies and practices that may dictate specific prerequisites and an authorization process prior to the release of products. Regional guidance on IVIg utilization management is provided by the BC Provincial Blood Coordinating Office, the Ontario Regional Blood Coordinating Network and the Atlantic Blood Utilization Strategy Working Group. The Prairie Collaborative Immune Globulin Utilization Management Framework Project developed criteria for the clinical use of immunoglobulin as part of an evidence-based framework to aid transfusion services and clinicians. The second edition was published in February 2022; Appendix C provides a list of new and revised recommendations.17
The COVID-19 pandemic heightened concerns about possible future shortages of IVIg. The National Advisory Committee on Blood and Blood Products (NAC) provides interim guidance on managing Ig shortages and a project is underway to build on this guidance to develop a national plan for managing Ig shortages18,19 Deliverables are expected for submission to the provincial and territorial ministries of health by March 31, 2024.
Contraindications
Most manufacturers state that IVIg is contraindicated for individuals with IgA deficiency who have anti-IgA antibodies, but these individuals may be successfully treated with SCIg therapy.20 There is no requirement to routinely test for IgA deficiency prior to IVIg therapy. There are also reports of patients with demonstrated anti-IgA IgG antibodies tolerating IVIg infusions.21 For patients who have had anaphylactic or multiple severe allergic reactions to IVIg previously, consideration may be given to the use of solvent-detergent treated products. In addition, one product, Privigen, recommends against use in patients with hyperprolinemia.
Dosing and administration
Dosing for IVIg infusion is dependent on the clinical indication. Generally, the immune replacement dose is 0.4–0.6 g/kg every 3–4 weeks. One additional dose of 0.4 g/kg may be given in the first month of therapy if the serum IgG level is markedly reduced. The immunosuppressive dose is 1–2 g/kg over 1–5 days, and some conditions may require ongoing maintenance therapy, usually given monthly, with efforts made to reduce the dose or extend the treatment interval based on the patient’s clinical response. Local practice guidelines, consensus documents and manufacturers’ product monographs provide more specific information on dose, frequency and duration of therapy for specific indications.
The NAC and several provincial health authorities and blood offices recommend IVIg dosing based on adjusted body weight calculators (e.g., Ontario,22Alberta,23 Nova Scotia,24 British Columbia25) and/or absolute dose caps. For additional details, refer to the online dose calculators provided and local policies. Figure 1 provides an example of an adjusted body weight dosing calculation.
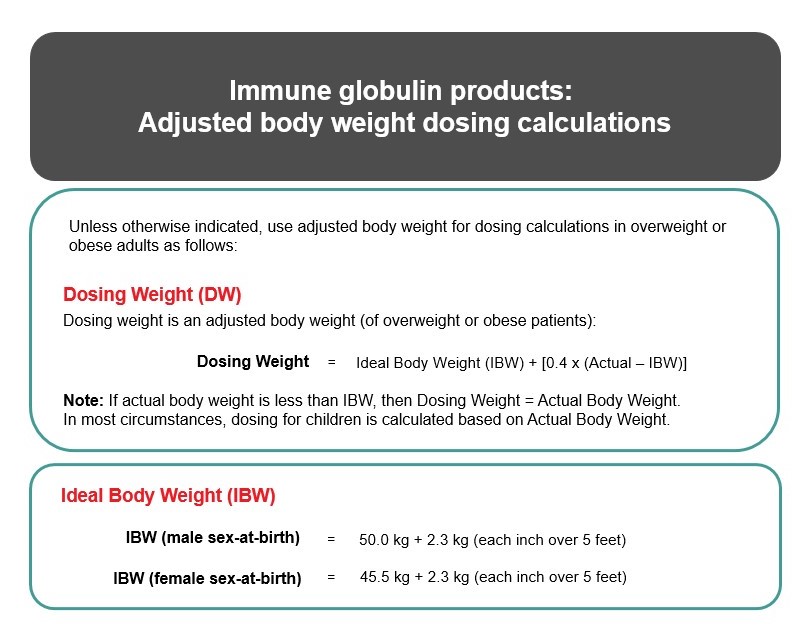
Figure 1. Example of an adjusted body weight dosing calculations.17 Ideal body weight is calculated using the Devine formula.26 In most circumstances, dosing for children is calculated based on Actual Body Weight.
IVIg must be administered intravenously at an infusion rate appropriate for the indication and specified by the ordering physician. Some reactions can be prevented or controlled in many cases by slowing the infusion rate.
Protocols for IVIg infusion vary by institution but are based on the following principles:
- Start with a slow infusion rate (e.g., 0.01 mL/kg/minute) and monitor vital signs frequently.
- As tolerated, increase the infusion rate at regular intervals with progressively less frequent monitoring of vital signs.
A patient’s response to the infusion will dictate an individualized maximum tolerable rate of infusion that may be lower than the manufacturer’s recommended infusion rate.
Storage
Storage temperatures range from 2–25°C but the product shelf life may differ with some products if stored at room temperature. Please consult each product monograph for the maximal allowable time at each temperature range.
Adverse events
The prevalence of IVIg-associated adverse events reported in the literature varies widely.27-30 Patients receiving immunoglobulin as supplementation for primary or secondary hypoglobulinemia appear to have a much lower frequency of side effects than do patients who are receiving higher IVIg doses as a treatment for immune-mediated or systemic inflammatory disorders.31
Minor side effects are quite common with IVIg infusion and are often related to infusion rate. These reactions include headache, chills, fever, malaise, anxiety, chest pain, nausea, pruritus, and rash. Most of these side effects will resolve by slowing or stopping the IVIg infusion. If recurrent, they can typically be managed by providing premedication or switching to an alternate product. The more serious and potentially fatal adverse events—including severe hemolysis, aseptic meningitis, anaphylaxis, viral transmission, transfusion-related acute lung injury (TRALI) and thromboembolic events—are rare. Since the implementation of donor testing and routine viral inactivation processes, the currently licensed products are considered safe with respect to transmission of human immunodeficiency virus (HIV) and the hepatitis viruses.32 Cases of IVIg-associated TRALI reactions have been reported and may be increasing as a result of TRALI mitigation strategies that divert plasma from donors with previous history of pregnancy (and potential for HLA sensitization) to fractionation processing.33,34
Hemolysis
IVIg administration commonly results in a positive direct antiglobulin test (DAT) and, in up to 32% of cases, contributes to clinically significant hemolytic events.35 IVIg-associated hemolysis has been defined by the IVIg Hemolysis Pharmacovigilance Group of Canada as:
- A drop in hemoglobin of at least 10 g/L and a positive DAT within 10 days following IVIg infusion with supporting evidence of hemolysis as indicated by at least two of:
- increased reticulocyte count
- increased lactate dehydrogenase level
- low haptoglobin level
- increased unconjugated bilirubin level
- hemoglobinemia (visibly red serum)
- hemoglobinuria
- or the presence of significant spherocytosis and no alternate etiology for the anemia.36
Many case series have described IVIg-associated hemolysis as having a higher occurrence rate in patients receiving high doses, especially at doses of 2 g/kg.35,37-39 The higher prevalence of IVIg-associated hemolysis in those with non-O blood groups occurs as a function of both the quantity of passively transferred anti-A and anti-B isohemagglutinins as well as the density of A and B antigens on the red cell surface of the recipient.35,40 Some manufacturers are now providing IVIg products that are isohemagglutinin-depleted to minimize risk. The risk of hemolysis appears highest when a product with a high isohemagglutinin titre is administered at doses of 2 g/kg or higher to a blood group A or AB recipient41 some Canadian jurisdictions have implemented prospective hemolysis monitoring processes for these patients.
Aseptic meningitis
Aseptic meningitis secondary to IVIg appears to be dose-related; the majority of reported cases received immunomodulatory doses of 2 g/kg/cycle.42 Meningeal signs and symptoms typically present within 6 to 48 hours of the infusion. On examination, the cerebrospinal fluid demonstrates elevated protein levels, normal to low glucose levels, and a leukocyte pleocytosis with negative cultures.43 The majority of patients recover within five days of symptom onset and tolerate subsequent infusions, but some patients report the recurrence of symptoms with subsequent infusions.44
Anaphylaxis
Severe anaphylactic and allergic reactions have been reported in association with IVIg. Some of these reactions have occurred in patients with IgA deficiency and anti-IgA antibodies but there is debate regarding the significance of IgG versus IgE anti-IgA, the role of complement activation, and the persistence of the reactivity.21,45,46 The use of SCIg may be one effective substitute in patients with a history of anaphylactic or severe allergic reactions who require future Ig therapy.20 Others recommend the use of IgA-depleted products in those with confirmed anti-IgA antibodies and prior confirmed reactions.47
Thromboembolic events
Health Canada and the US Food and Drug Administration (FDA) have both issued safety warnings regarding the potential of thromboembolic complications with Ig products.48,49 Reported thromboembolic complications include stroke, transient ischemic attacks, deep vein thromboses, pulmonary emboli, retinal vein occlusion, and retinal artery infarcts. These thrombotic complications can occur during the IVIg infusion or up to eight days following.50 Patients with cardiovascular risk factors, advanced age, prolonged immobilization and those with a history of thromboembolic events are considered at a higher risk, although thrombosis may occur in the absence of any identifiable risk factors. High-risk patients should be carefully monitored and adequately hydrated prior to the IVIg administration. The Ig products should also be administered at the lowest feasible dose and an infusion rate appropriate for the indication and patient condition.
Subcutaneous immunoglobulin
In Canada, subcutaneous immunoglobulin (SCIg) is predominantly used as replacement therapy for primary and secondary immunodeficiency patients. Since these patients require lifelong therapy with Ig replacement, many may have better quality of life parameters with SCIg use instead of IVIg. These benefits includes improved side effect profile given no need for vascular access, increased convenience due to self-administered home infusions and fewer restrictions in travel.51 As it pertains to decreasing the frequency and duration of infection in patients with primary immune deficiency, SCIg and IVIg are considered equally effective.52 As with any blood product managed at home, the use of SCIg should be overseen by a comprehensive care clinic that provides training for patients and caregivers in administration, proper handling, storage and monitoring for adverse effects.
Indications
The licensed indication for SCIg includes both replacement therapy for primary and secondary immunodeficiency as well as for immunomodulation in patients with the neurologic condition chronic inflammatory demyelination polyneuropathy (CIDP). Home/self-administration of SCIg is a safe, effective and preferred approach for many people offering increased quality of life and reduced risk of adverse reactions.53,54
Contraindications
The main contraindication for SCIg is a history of anaphylactic or severe allergic reactions to Ig preparations. However, this is often a reason for switching a patient from intravenous to subcutaneous products. Some, but not all, products advise against use in those with a history anti-IgA antibodies. One product, Hizentra, recommends against use in patients with hyperprolinemia.
Dose and administration
For initiation of replacement therapy in patients with primary immunodeficiency, SCIg starting dose depends on the specific brand being used. Generally, the doses vary between 100–200 mg/kg per week depending on the product used The recommended rate of infusion varies by brand.55-57 One additional dose of 0.4 g/kg may be given in the first month of therapy if the serum IgG level is markedly reduced.
If transitioning from IVIg, the easiest calculation is to take the monthly total IVIg dose and divide by 4 to obtain the weekly SCIg dose followed by titration to achieve an IgG trough level of at least the lower limit of the age-specific serum IgG reference range, or as needed to achieve clinical effectiveness.58
One SCIg product, HyQvia, approved for primary and secondary immunodeficiency, may be administered once monthly. It is administered along with hyaluronidase, which allows a larger volume of Ig to be injected. The usual dose is 100-125 mg/kg per week, which may begin as weekly doses then be given cumulatively every 3 to 4 weeks.
For immunomodulation therapy in CIDP, the only licensed SCIg is Hizentra and the monograph recommends dosing between 200 to 400 mg/kg per week.56
Storage
Storage temperatures range from 2–25°C but product shelf life may differ with some products if stored at room temperature. For products that should be stored in the fridge until administered to the patient, the date the product was removed from the fridge should be noted. Depending on the product specifications, some products may be stored at room temperature in the patient’s home. Please consult each product monograph for maximal time at each temperature range.
Adverse events
The minor adverse event profile with SCIg is similar to that of IVIg, with the additional side effect of discomfort from subcutaneous injection. Please refer to the above section on adverse events for IVIg.
The BC Provincial Blood Coordinating Office (PBCO), in collaboration with immunologists and transfusion medicine physicians, and with support from Canadian Blood Services’ BloodTechNet program, developed a Primary Immunodeficiency Disease (PIDD) toolkit to support the diagnosis, treatment and monitoring of patients with primary immunodeficiency disease (PIDD). The toolkit contains diagnostic and treatment algorithms, a dose calculator to determine IVIg or SCIg dose, a dose adjustment calculator and links to references of interest.
Hyperimmune globulins
Hyperimmune globulin fractionation products are created from pools of human plasma specifically chosen for high titres of antibodies with selected specificities. Each product undergoes viral inactivation procedures but the process used is dependent on the individual manufacturer.
Contraindications
- IgA deficiency
- Previous severe or allergic reaction to the product
- Any condition that would contraindicate intramuscular injections
Rh Immunoglobulin
Rh immunoglobulin (RhIg) is a freeze-dried preparation of human immunoglobulin of the IgG class with antibody specificity directed against the RhD antigen. This product is prepared from pooled human plasma collected from paid donors who selectively produce anti-D.59,60 RhIg is not antigen affinity-purified and can be expected to contain background levels of some other IgG antibodies. Although most RhIg products have high purity without high levels of complement activity, some products will contain residual antibodies against other Rh antigens.
Product description
The available vial sizes include: 600 IU (120 µg), 1,500 IU (300 µg) and 5,000 IU (1,000 µg) anti-D. See the package insert for additional product-specific details. See Chapter 12, Hemolytic disease of the fetus and newborn and perinatal immune thrombocytopenia, for more information on RhIg.
Clinical use61-63
There are two broad categories for clinical use of RhIg: prevention of alloimmunization to the RhD antigen (see Table 2) and for treatment of immune thrombocytopenic purpura (see Table 3).
Table 2: RhIg for prevention of alloimmunization to the RhD antigen: indications, contraindications and dose and administration
| Category 1: Prevention of alloimmunization to the RhD antigen | |
|---|---|
| Indications |
|
| Contraindications |
|
| Dose and administration |
|
Table 3: RhIg for the treatment of immune thrombocytopenic purpura: indications, contraindications and dose and administration
| Category 2: Immune thrombocytopenic purpura | |
|---|---|
| Indications | Administration of RhIg for ITP differs from its other uses in that the patient must be RhD-positive and must have an intact and functional spleen. |
| Contraindications |
|
| Dose and administration |
|
Hepatitis B immunoglobulin
Hepatitis B Immune Globulin is a sterile solution of the purified IgG fraction of human plasma containing antibodies to hepatitis B surface antigen (anti-HBs). Hepatitis B Immune Globulin is manufactured from plasma collected from healthy, screened donors with high titres of anti-HBs.
Table 4: Hepatitis B immunoglobulin for providing passive immunization65
| Indications |
To provide passive immunization to hepatitis B in the following situations:
|
| Contraindications | 0.06 mL/kg given IM or 0.5 mL for infants as soon as possible, preferably < 24 hours |
Other hyperimmunoglobulins
Indications and dose and administration for other hyperimmune globulin fractionation products carried on the Canadian Blood Services product formulary are provided in Table 5. Please refer to the product monograph for specific dosing recommendations for each specific disease exposure.
Table 5: Other hyperimmunoglobulin fractionation products on the Canadian Blood Services product formulary.
| Product name | Indication | Dose and administration |
|---|---|---|
|
Varicella-Zoster Immune Globulin (VariZIG) |
Prevention or reduction in severity of maternal infections in pregnant women that have had a significant exposure to the varicella zoster virus (VZV) providing that the exposed individual does NOT have known immunity to the varicella zoster virus (secondary to either vaccination or previous infection).66 |
The recommended adult dose is 125 IU/10 kg body weight up to a maximum dose of 625 IU. Each vial contains approximately 125 IU of anti-VZV. VariZIG can be given by intravenous (IV) or intramuscular (IM) administration. VariZIG should be administered as soon as possible but at least within 96 hours of exposure. However, the efficacy after this time frame has not been established. |
|
Intramuscular Immune Globulin (GamaSTAN S/D) |
Passive immunization using IMIg may be considered for immediate post exposure prophylaxis when vaccines for active immunization are not available or are contraindicated due to the exposed individual’s age or underlying medical condition. |
GamaSTAN S/D is administered intramuscularly preferably in the anterolateral aspects of the upper thigh and the deltoid muscle of the upper arm. The gluteal region should not be used routinely as an injection site because of the risk of injury to the sciatic nerve. Dosing recommendations differ for different indications. Please refer to product monograph or Canadian Immunization Guide. Doses over 10 mL should be divided and injected into several muscle sites to reduce local pain and discomfort. |
|
Cytomegalovirus Immunoglobulin (Cytogam) |
Cytomegalovirus (CMV) Immunoglobulin Intravenous (Human) is primarily indicated for solid organ transplant recipients who are seronegative for CMV but are receiving an organ from a CMV seropositive donor to mitigate the development of primary (1°) CMV disease. In transplants of organs other than kidneys, concomitant therapy with ganciclovir may be administered. Of note, in Canada, Cytogam is only approved for use in Kidney transplant. |
The maximum recommended total dosage per infusion is 150 mg/kg. The product should be administered intravenously according to the following schedule but should not exceed a rate of:
|
Storage
The storage temperature ranges from 2–8ºC. The product must be used within four hours of reconstitution.
Adverse events
WinRho SDF (Anti-D IG) RhIg has a serious warning and precautions label regarding the risk of severe hemolysis when used for immune thrombocytopenic purpura – see contraindications above. Otherwise, the adverse event profile is similar to that of other immunoglobulins.
Continuing professional development credits
Fellows and health-care professionals who participate in the Canadian Royal College's Maintenance of Certification (MOC) program can claim the reading of the Clinical Guide to Transfusion as a continuing professional development (CPD) activity under Section 2: Individual learning. Learners can claim 0.5 credits per hour of reading to a maximum of 30 credits per year.
Medical laboratory technologists who participate in the Canadian Society for Medical Laboratory Science’s Professional Enhancement Program (PEP) can claim the reading of the Clinical Guide to Transfusion as a non-verified activity.
Acknowledgements
The authors, Sheila Rutledge Harding, MD, MA, FRCPC; Juthaporn Cowan, MD, PhD,FRCPC, FACP; and Sarah Jennings, RPh, PharmD; acknowledge Kathryn Webert, MD, MSc, FRCPC; for her review of this chapter.
Suggested citation
Rutledge Harding S, Cowan J, Jennings S. Immunoglobulin products. In: Khandelwal A, Abe T, editors. Clinical Guide to Transfusion [Internet]. Ottawa: Canadian Blood Services, 2022 [cited YYYY MM DD]. Chapter 4. Available from: https://professionaleducation.blood.ca
If you have questions about the Clinical Guide to Transfusion or suggestions for improvement, please contact us through the Feedback form.
References
- Government of Canada. Blood products, human immunoglobulin and timing of immunization: Canadian Immunization Guide. Vol. 2023 (Government of Canada, 2023).
- Gelfand, E. Differences between IVIG products: impact on clinical outcome. Int Immunopharmacol 6, 592-599 (2006).
- National Advisory Committee on Blood and Blood Products. NAC Statement on clinical equivalency of select fractionated plasma protein products. (2022).
- Lu, H., Lok, A.S., Warneke, C.L., et al. Passive transfer of anti-HBc after intravenous immunoglobulin administration in patients with cancer: a retrospective chart review. The Lancet. Haematology 5, e474-e478 (2018).
- Suresh, J. & Kyle, B.D. Clinical false positives resulting from recent intravenous immunoglobulin therapy: case report. BMC Infect Dis 21, 288 (2021).
- Crow, A.R. & Lazarus, A.H. Mechanistic properties of intravenous immunoglobulin in murine immune thrombocytopenia: support for FcgammaRIIB falls by the wayside. Seminars in hematology 53 Suppl 1, S20-22 (2016).
- Samuelsson, A., Towers, T. & Ravetch, J. Anti-inflammatory Activity of IVIG Mediated Through the Inhibitory Fc Receptor. Science 291, 484-486 (2001).
- Crow, A., Song, S., Semple, J., et al. IVIg inhibits reticuloendothelial system function and ameliorates murine passive-immune thrombocytopenia independent of anti-idiotype reactivity. British Journal of Haematology 115, 679-686 (2001).
- Keller, M.A. & Stiehm, E.R. Passive immunity in prevention and treatment of infectious diseases. Clin Microbiol Rev 13, 602-614 (2000).
- Winau, F. & Winau, R. Emil von Behring and serum therapy. Microbes Infect 4, 185-188 (2002).
- Kazatchkine , M.D. & Kaveri , S.V. Immunomodulation of Autoimmune and Inflammatory Diseases with Intravenous Immune Globulin. New England Journal of Medicine 345, 747-755 (2001).
- Samuelsson, A., Towers, T.L. & Ravetch, J.V. Anti-inflammatory Activity of IVIG Mediated Through the Inhibitory Fc Receptor. Science 291, 484-486 (2001).
- Tankersley, D.L. Dimer formation in immunoglobulin preparations and speculations on the mechanism of action of intravenous immune globulin in autoimmune diseases. Immunol Rev 139, 159-172 (1994).
- Larroche, C., Chanseaud, Y., Garcia de la Pena-Lefebvre, P., et al. Mechanisms of intravenous immunoglobulin action in the treatment of autoimmune disorders. BioDrugs 16, 47-55 (2002).
- Galeotti, C., Kaveri, S.V. & Bayry, J. IVIG-mediated effector functions in autoimmune and inflammatory diseases. Int Immunol 29, 491-498 (2017).
- Canada, G.o. Final report of the Expert Panel on Immune Globulin Product Supply and Related Impacts in Canada. (ed. Canada, H.) (2018).
- Prairie Collaborative Immune Globulin Utilization Management Framework Project. Criteria for the clinical use of immune globulin. (Alberta Ministry of Health, Shared Health Manitoba, and Saskatchewan Ministry of Health, 2022).
- National Advisory Committee on Blood and Blood Products. National Ig Shortages management Plan: Project Overview. (2023).
- Canadian Blood Services and National Advisory Committee on Blood and Blood Products. The national plan for management of shortages of immnoglobulin products (Ig) - Interim guidance. (2020).
- Eijkhout, H.W., van den Broek, P.J. & van der Meer, J.W. Substitution therapy in immunodeficient patients with anti-IgA antibodies or severe adverse reactions to previous immunoglobulin therapy. Neth J Med 61, 213-217 (2003).
- Rachid, R., Castells, M., Cunningham-Rundles, C., et al. Association of anti-IgA antibodies with adverse reactions to gamma globulin infusion. The Journal of allergy and clinical immunology 128, 228-230.e221 (2011).
- Ontario Regional Blood Coordinating Network. IVIG dose calculator.
- Alberta Health Services. IVIG Dosing based on Adjusted Body Weight Calculation. (2018).
- Nova Scotia Provincial Blood Coordinating Program. IVIG Dose Calculator. (2017).
- The BC IVIG Utilization Management Program. IVIG Dosing based on Adjusted Body Weight Calculation. (BC Provincial Blood Coordinating Office).
- Devine, B.J. Gentamicin therapy. Drug intelligence and clinical pharmacy 8, 650-655 (1974).
- Bertorini, T.E., Nance, A.M., Horner, L.H., et al. Complications of intravenous gammaglobulin in neuromuscular and other diseases. Muscle Nerve 19, 388-391 (1996).
- Brennan, V., SalomÉ-Bentley, N. & Chapel, H. Prospective audit of adverse reactions occurring in 459 primary antibody-deficient patients receiving intravenous immunoglobulin. Clinical and Experimental Immunology 133, 247-251 (2003).
- Katz, U., Achiron, A., Sherer, Y., et al. Safety of intravenous immunoglobulin (IVIG) therapy. Autoimmunity Reviews 6, 257-259 (2007).
- Nahirniak, S., Blain, H. & Clarke, G. IVIG associated adverse outcomes- comparison to monograph rates and product type. Transfusion 53, SP211 (2013).
- Cherin, P., Marie, I., Michallet, M., et al. Management of adverse events in the treatment of patients with immunoglobulin therapy: A review of evidence. Autoimmun Rev 15, 71-81 (2016).
- Schiff , R. Transmission of Viral Infections through Intravenous Immune Globulin. New England Journal of Medicine 331, 1649-1650 (1994).
- Quest, G., Gaal, H., Clarke, G., et al. Transfusion-related acute lung injury after transfusion of pooled immune globulin: a case report. Transfusion 54, 3088-3091 (2014).
- Rizk, A., Gorson, K., Kenney, L., et al. Transfusion-related acute lung injury after the infusion of IVIG. Transfusion 41, 264-268 (2001).
- Pendergrast, J., Armali, C., Callum, J., et al. A prospective observational study of the incidence, natural history, and risk factors for intravenous immunoglobulin-mediated hemolysis. Transfusion 61, 1053-1063 (2021).
- Health Canada. ARCHIVED - Canadian Adverse Reaction Newsletter, Volume 19, Issue 4, October 2009.
- Wilson, J., Bhoopalam, N. & Fisher, M. Hemolytic anemia associated with intravenous immunoglobulin. Muscle & Nerve 20, 1142-1145 (1997).
- Daw, Z., Padmore, R., Neurath, D., et al. Hemolytic transfusion reactions after administration of intravenous immune (gamma) globulin: a case series analysis. Transfusion 48, 1598-1601 (2008).
- Kahwaji, J., Barker, E., Pepkowitz, S., et al. Acute Hemolysis After High-Dose Intravenous Immunoglobulin Therapy in Highly HLA Sensitized Patients. Clinical Journal of the American Society of Nephrology 4, 1993-1997 (2009).
- Branch, D.R., Hellberg, A., Bruggeman, C.W., et al. ABO zygosity, but not secretor or Fc receptor status, is a significant risk factor for IVIG-associated hemolysis. Blood 131, 830-835 (2018).
- Bellac, C., Hottiger, T., Jutzi, M., et al. The role of isoagglutinins in intravenous immunoglobulin–related hemolysis. Transfusion 55, S13-S22 (2015).
- Sekul, E., Chow, C. & Dalakas, M. Magnetic resonance imaging of the forearm as a diagnostic aid in patients with sporadic inclusion body myositis. Neurology 48, 863-866 (1997).
- Scribner, C.L., Kapit, R.M., Phillips, E.T., et al. Aseptic Meningitis and Intravenous Immunoglobulin Therapy. Annals of internal medicine 121, 305-306 (1994).
- Kato, E., Shindo, S., Eto, Y., et al. Administration of immune globulin associated with aseptic meningitis. JAMA 259, 3269-3271 (1988).
- de Albuquerque Campos, R., Sato, M. & da Silva Duarte, A. IgG anti-IgA subclasses in common variable immunodeficiency and association with severe adverse reactions to intravenous immunoglobulin therapy. Journal of clinical immunology 20, 77-82 (2000).
- Burks , A., Sampson , H. & Buckley , R. Anaphylactic Reactions after Gamma Globulin Administration in Patients with Hypogammaglobulinemia. New England Journal of Medicine 314, 560-564 (1986).
- Cunningham-Rundles, C., Zhou, Z., Mankarious, S., et al. Long-term use of IgA-depleted intravenous immunoglobulin in immunodeficient subjects with anti-IgA antibodies. Journal of clinical immunology 13, 272-278 (1993).
- Health Canada. ARCHIVED - Canadian Adverse Reaction Newsletter, Volume 18, Issue 1, January 2008.
- U.S. Food and Drug Administration. FDA Safety Communication: New boxed warning for thrombosis related to human immune globulin products - November 14, 2013. (2013).
- Marie, I., Maurey, G., Hervé, F., et al. Intravenous immunoglobulin-associated arterial and venous thrombosis; report of a series and review of the literature. British Journal of Dermatology 155, 714-721 (2006).
- Chapel, H., Spickett, G., Ericson, D., et al. The comparison of the efficacy and safety of intravenous versus subcutaneous immunoglobulin replacement therapy. Journal of Clinical Immunoematology 20, 94-100 (2000).
- Shehata, N., Palda, V., Bowen, T., et al. The use of immunoglobulin therapy for patients with primary immune deficiency: an evidence-based practice guideline. Transfusion medicine reviews 24 Suppl 1, S28-50 (2010).
- Racosta, J.M., Sposato, L.A. & Kimpinski, K. Subcutaneous versus intravenous immunoglobulin for chronic autoimmune neuropathies: A meta-analysis. Muscle Nerve 55, 802-809 (2017).
- Goyal, N.A., Karam, C., Sheikh, K.A., et al. Subcutaneous immunoglobulin treatment for chronic inflammatory demyelinating polyneuropathy. Muscle Nerve 64, 243-254 (2021).
- Government of Canada. Product information, Cutaquig. Vol. 2023 (Government of Canada, 2023).
- Government of Canada. Product information, Hizentra. Vol. 2023 (Government of Canada, 2023).
- Government of Canada. Product information, Cuvitru. Vol. 2023 (Government of Canada, 2023).
- Krishnarajah, G., Lehmann, J.K., Ellman, B., et al. Evaluating dose ratio of subcutaneous to intravenous immunoglobulin therapy among patients with primary immunodeficiency disease switching to 20% subcutaneous immunoglobulin therapy. Am J Manag Care 22, s475-s481 (2016).
- Mayekar, R.V., Paradkar, G.V., Bhosale, A.A., et al. Recombinant anti-D for prevention of maternal-foetal Rh(D) alloimmunization: a randomized multi-centre clinical trial. Obstet Gynecol Sci 63, 315-322 (2020).
- Kent, J., Farrell, A.-M. & Soothill, P. Routine administration of Anti-D: the ethical case for offering pregnant women fetal RHDgenotyping and a review of policy and practice. BMC Pregnancy and Childbirth 14, 87 (2014).
- White, J., Qureshi, H., Massey, E., et al. Guideline for blood grouping and red cell antibody testing in pregnancy. Transfusion medicine (2016).
- Qureshi, H., Massey, E., Kirwan, D., et al. BCSH guideline for the use of anti-D immunoglobulin for the prevention of haemolytic disease of the fetus and newborn. Transfusion medicine 24, 8-20 (2014).
- BCSH Anti-D Guidelines 2014 - Amendment 4.8.14. BCSH Guidelines.
- Meyer, O., Kiesewetter, H., Hermsen, M., et al. Replacement of intravenous administration of anti-D by subcutaneous administration in patients with autoimmune thrombocytopenia. Pediatric blood & cancer 47, 721-722 (2006).
- Government of Canada. Hepatitis B vaccines: Canadian Immunization Guide, for health professionals. Vol. 2023 (Public Health Agency of Canada, 2023).
- Government of Canada. Varicella (chickenpox) vaccines: Canadian Immunization Guide. Vol. 2023 (Government of Canada, 2023).