Blood system inventory management best practices guide
Authors: Gwen Clarke, MD, FRCPC; and Rob Romans, ART, BSc
Online publication date: August 2020
Also available as a PDF and at blood.ca
Primary target audiences: Medical laboratory technologists (MLT) and MD in a hospital transfusion laboratory
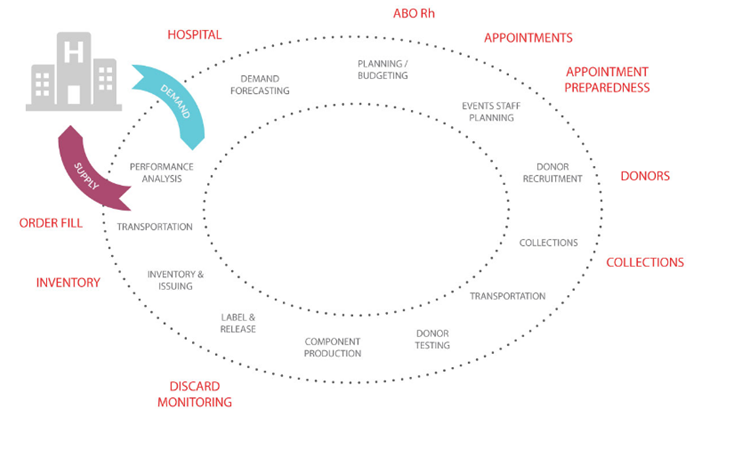
Blood is a resource that must be carefully managed to ensure that each donation is used to provide the best possible benefit to patients. Blood operators are responsible for providing a safe, secure and cost-effective supply of blood components, products, and services. Effective inventory management is the collective responsibility of all blood system stakeholders.
Adherence to system-wide inventory management best practices can optimize donor collections, component manufacturing, and the inventory that a blood supplier and a hospital needs to keep on hand to meet patient needs, and contribute to minimizing component outdate rates.
Data are essential for effective inventory management. Hospitals share disposition data (monthly) and inventory levels (best is daily) with Canadian Blood Services. These data are used to generate a graphical tool to present the hospital’s actual red blood cell inventory over time in comparison to their average daily red cell demand (ADRD) plotted as usage over time. The graphical tool also calculates the actual inventory index (II), that can be used to effectively manage a hospital’s inventory. Hospitals are encouraged to report their inventory by ABO/Rh to enable the greatest benefit from the ADRD graph.
Definitions:
Red Cell Demand
#RBC transfused + #RBC outdated + #RBC wasted (all in-date discards)
ADRD
Red Cell Demand ÷ #days
Inventory Index
Inventory Level ÷ ADRD
For more details, please visit the National Advisory Committee on Blood and Blood Products (NAC), and review their National Blood Shortage Plan. The NAC collaborates with and provides advice on the utilization management of blood and blood products and transfusion medicine practice to the provincial and territorial (PT) Ministries of Health and Canadian Blood Services.
The following “vein to vein” blood system inventory management best practices are divided into sections based on the group responsible for the practice.
A. Blood Manufacturers/Suppliers
B. Hospital Transfusion Services/Blood Banks
Note: Implementation of some of the following recommendations may require prior consultation with the local provincial blood program, blood manufacturer/supplier or hospital transfusion service/blood bank management representative, hospital medical director, or hospital transfusion committee.
A. Blood Manufacturer / Blood Supplier
1. Conduct regular hospital demand forecasting that considers historical demand trends, environmental scans, clinical trends, as well as hospital customer specific operational changes that could impact demand. Demand forecasts provide the lead time necessary to ensure that supply is available to meet demand.
2. Establish blood collection targets based on the results of a demand forecast. Consider that hospital demand may be seasonal, and adjust collection and production targets accordingly.
3. Gather intelligence at regular intervals and review and adjust demand forecasts and collection targets as required. Agility is essential to consistently meet patient’s needs while operating a cost-effective service.
4. Review collection and manufacturing discard data on a regular basis, and implement targeted continuous process improvement  plans to reduce discards.
plans to reduce discards.
5. Collect hospital disposition data on a regular basis to determine the final disposition of all blood components and products. Knowing what blood components and plasma protein products are used by each hospital will improve the accuracy of demand forecasts. Disposition data that includes hospital discards facilitates discussions with hospital customers about optimal inventory levels and routine blood delivery schedules. Balancing blood system inventory levels, discard rates, and delivery frequency is critical to operating a cost-effective service.
6. Develop a blood system-wide, real time, inventory monitoring tool that provides visibility of blood component levels for all stakeholders. Establish inventory level categories for all blood components and ABO/Rh(D) blood group. Example inventory level categories are Excess, Optimal, Minimum, and Emergency, or Green, Amber, and Red.
7. Develop a tool to guide daily manufacturing plans, with defined targets for each component type by ABO/Rh(D) blood group that considers current inventory levels.
8. Conduct daily inventory management meetings. Multi-site blood suppliers should conduct daily inventory management meetings with all sites to communicate local demand challenges and facilitate inventory movement as required to best meet patient requirements and minimize discards.
9.  Share inventory levels daily with hospital customers to promote system-wide visible inventory levels, and establish a process for promptly notifying hospitals customers of any inventory challenges.
Share inventory levels daily with hospital customers to promote system-wide visible inventory levels, and establish a process for promptly notifying hospitals customers of any inventory challenges.
10. Establish a blood shortage plan in collaboration with all stakeholders that includes participant actions resulting from supply disruptions and/or disasters. Conduct mock exercises to ensure the plan will function as expected, and update the plan to reflect evolving scenarios.
11. Arrange “released” inventory to ensure that oldest (shortest remaining shelf life) are at the front of the storage unit. Alert staff to inventory with short outdates to help ensure they will be issued to hospital customers first. Post a list on the storage unit or tag the components/products as a visible cue.
12. Maintain a segregated stock, in labeled bins (or use tags or a Kanban system), of antigen negative RBCs. If a hospital has a patient(s) on a regular transfusion schedule who requires antigen negative RBCs, keep a segregated stock for such patients.
13. Avoid providing a large number of components with the same expiry date when filling hospital customer orders (e.g. >10 components of the same blood component type and blood group). Managing large numbers of components all expiring on the same day can be challenging for hospital customers. Other considerations may be appropriate for smaller, more distant hospital customers.
14.  Establish delivery schedules in collaboration with hospital customers. Establish definitions for blood order delivery priorities (e.g. Routine, ASAP, STAT). Review frequency of non-routine requests on a regular basis and explore opportunities to adjust inventory levels to optimize such deliveries.
Establish delivery schedules in collaboration with hospital customers. Establish definitions for blood order delivery priorities (e.g. Routine, ASAP, STAT). Review frequency of non-routine requests on a regular basis and explore opportunities to adjust inventory levels to optimize such deliveries.
B. Hospital Transfusion Service / Blood Bank
1. Determine target inventory levels and maintain these levels by using an “stock up” policy. Rule of thumb is to maintain a stock  inventory of the equivalent to approximately 4-6 days of average daily use of red blood cells (RBCs) and 2 days of average daily use of platelets (based on averaging annual use divided by the number of days when most blood is used). Inventory calculators can provide a rough estimate. Inventory levels and average daily red cell demand (ADRD) should be reviewed at least annually, and when blood utilization practices change at the hospital, the target inventory levels should be revised as needed. Additional considerations:
inventory of the equivalent to approximately 4-6 days of average daily use of red blood cells (RBCs) and 2 days of average daily use of platelets (based on averaging annual use divided by the number of days when most blood is used). Inventory calculators can provide a rough estimate. Inventory levels and average daily red cell demand (ADRD) should be reviewed at least annually, and when blood utilization practices change at the hospital, the target inventory levels should be revised as needed. Additional considerations:
- Review pre-admission and next day’s surgical schedule to ensure blood group specific units are available.
- Adjust inventory target levels if significant seasonal demand fluctuations occur, such as areas with seasonal residents and/or tourists.
- Define and review target inventory levels for all components/products.
- Identify target inventory levels as part of a hospital emergency blood management plan.
- Align with definitions provided in provincial or national emergency blood management plans.
2. Arrange inventory to ensure the oldest (shortest remaining shelf life) are at the front of the storage shelf. Alert staff to units that will be outdating soon (e.g. RBC in the next 5 days, platelets same day, plasma protein products and frozen products in next 3 months) to help ensure they will be used first. Use visual aids such as an expiring units list on the storage unit or place distinctive tags on the units. Ensure that a strict ‘oldest unit first out’ policy is adhered to, unless standard operating procedures dictate specific requirements for certain patient groups. Include reserved units (which may be kept in a separate area) in this process by moving them into useable inventory before they reach the end of their shelf life.
3. Hold approximately 6-9 per cent of inventory as K negative, to meet the needs of women of child bearing potential. Studies have defined child bearing potential as female patients who are 45 years of age or younger. For most general adult hospitals, less than 10 per cent of transfusions are directed to female patients of child bearing potential. For the five pediatric hospitals served by Canadian Blood Services, we recommend holding 50 per cent of inventory as K negative.
Some hospital laboratory information systems (LIS) can provide an alert to staff if a patient meets the recommendations to receive K negative RBCs. Explore this option with the LIS provider.
4. Maintain a segregated antigen negative RBC stock in labeled bins, or use tags or a similar Kanban system. If bins are used, consider color coding to assist staff with appropriate unit selection. Base stock held on hospital patient population. Approximately 3 per cent of hospital patients have clinically significant RBC antibodies. For those that do have a clinically significant RBC antibody, the most common are anti-D, anti-E, anti-c, and anti-K.
Below are some inventory recommendations based on number of RBC transfusions per year. These are only suggested starting points that may need to be adjusted up or down. Other antigen negative ABO blood groups can be ordered on demand as required for individual patients.
- Rotate segregated inventory into routine inventory regularly.
- Overstocking may result in RBCs not being readily available for patients with RBC antibodies in other hospitals.
- These recommendations may not be applicable to hospital sites who receive crossmatched red blood cell units from an affiliated/centralized transfusion testing laboratory.
| Hospital Size / Type | Starting Recommendation | Comments |
|---|---|---|
|
Transfuse >6000 RBCs/year
Image
 |
Group O 6 units c, E, K negative, Rh(D) positive 2 units c, E, K, Jka negative, Rh(D) positive 1 unit C, e, K negative, Rh(D) positive 2 units Jka negative, Rh(D) positive 3 units K negative, Rh(D) negative
Group A 4 units c, E, K negative, Rh(D) positive 2 units c, E, K, Jka negative, Rh(D) positive 1 unit C, e, K negative, Rh(D) positive 2 units Jka negative, Rh(D) positive 3 units K negative, Rh(D) negative
Group B 2 units c, E, K negative, Rh(D) positive |
Units negative for other antigens may be held for known patients in your community. Hospitals with a hemoglobinopathy program, hub hospitals, or those that transfuse >10,000 RBCs per year may choose to augment their antigen negative inventory. |
|
Transfuse 3000-5999 RBCs/year
Image
 |
Group O 2 units c, E, K negative, Rh(D) positive 1 unit c, E, K, Jka negative, Rh(D) positive 1 unit Jka negative, Rh(D) positive 2 units K negative, Rh(D) negative
Group A 2 units c, E, K negative, Rh(D) positive 1 unit c, E, K, Jka negative, Rh(D) positive 1 unit Jka negative, Rh(D) positive 2 units K negative, Rh(D) negative |
Units negative for other antigens may be held for known patients in your community. Hospitals with a hemoglobinopathy program or hub hospitals may choose to augment their antigen negative inventory. |
|
Transfuse 1000-2999 RBCs/year
Image
 |
Group O 2 units c, E, K negative, Rh(D) positive 2 units C, E, K negative, Rh(D) negative Group A 2 units c, E, K negative, Rh(D) positive 2 units C, E, K negative, (Rh(D) negative |
Units negative for other antigens may be held for known patients in your community. |
|
Transfuse 200-999 RBCs/year
Image
|
Group O 1 unit c, E, K negative Rh(D) positive 1 unit C, E, K negative, Rh(D) negative Group A 1 unit c, E, K negative, Rh(D) positive 1 unit C, E, K negative, Rh(D) negative |
Units negative for other antigens may be held for known patients in your community. |
|
Transfuse <199 RBCs/year
Image
|
Unless you have a patient in your community who has an ongoing need for antigen negative RBCs, we do not recommend holding antigen negative inventory (other than K negative RBCs for women of child-bearing potential). |
5. Perform an inventory count prior to placing a “stock up” order with the blood supplier. Ensure that the inventory count includes any stock that is held in remote locations such as emergency rooms or operating rooms, and includes a regular verification between computer inventory count and a physical count.
6. Implement policies to address the management of group O Rh(D) negative RBCs to preserve these lower incidence blood components. These policies should include reserving them for female patients of child bearing potential and children. The use of O Rh(D) negative RBC for non-O Rh(D) negative recipients should be minimized wherever possible. This practice should be monitored and reviewed regularly to ensure inventory levels are kept at optimum levels to avoid wastage and to ensure there is a sufficient supply for those patients who really need them.
7. Limit crossmatch/reserve inventory. Use of electronic or immediate spin crossmatch techniques can aid in reducing the length of time units remain on hold for a patient. Regular review and return to available inventory as soon as possible (within 24 hours) will reduce the number of units being held. For surgical patients, a review of the patient’s surgical blood use, the most recent post-operative hemoglobin result, and the presence of any clinically significant alloantibodies may assist with the decision.
8.  Establish a maximum surgical blood order schedule (MSBOS). A MSBOS is based on a hospital’s past RBC use and serves as a guideline for future surgical and other RBC transfusion requests. A MSBOS can guide ordering practice and avoid “just in case” ordering.
Establish a maximum surgical blood order schedule (MSBOS). A MSBOS is based on a hospital’s past RBC use and serves as a guideline for future surgical and other RBC transfusion requests. A MSBOS can guide ordering practice and avoid “just in case” ordering.
Note: Endorsement by a hospital’s transfusion committee, communication of the MSBOS guidelines to hospital physicians, surgeons, and nurse practitioners, and regular review of the MSBOS guidelines are critical to its success. Crossmatch requests that exceed the MSBOS guidelines may require consultation. The use of pre-printed order sets can also improve ordering practices.
9.  Implement redistribution to minimize outdates. Smaller hospitals should consider an arrangement to transfer “soon to outdate” blood components and products to a nearby larger hospital with a higher demand. Packing procedures must ensure the blood components/products are maintained at the appropriate conditions during transport and that the appropriate documentation accompanies the transfer.
Implement redistribution to minimize outdates. Smaller hospitals should consider an arrangement to transfer “soon to outdate” blood components and products to a nearby larger hospital with a higher demand. Packing procedures must ensure the blood components/products are maintained at the appropriate conditions during transport and that the appropriate documentation accompanies the transfer.
10. Staff training and awareness can contribute to improved inventory management practices. Provide clear standard operating procedures and ensure staff understands the importance and value of the blood components and products to minimize wastage. Having experienced staff perform the inventory count and ordering can minimize variability in practice, which will contribute to better overall inventory management and control.
11. Collaborate with clinical staff. This can make a significant difference in improving component/product ordering practices. Screening of orders, audits, guidelines and consultation with a transfusion medicine physician can help reduce unnecessary or inappropriate ordering of blood. Increasing awareness of the value of blood components and products, timelines for availability, and the risks involved with transfusion can also improve practice and minimize wastage.
12. Avoid large numbers of units expiring on the same day. When replacing large stock orders for one blood type, ask the blood supplier to send units with a mixture of expiry dates. Trying to manage large numbers of components all expiring on the same day can be challenging.
Posters provided as additional resources
1. Hospital Inventory Management Best Practices Poster
2. Blood Inventory Management Best Practices Poster
References
- Age of Child-Bearing Potential for Ontario Women in 2016; http://transfusionontario.org/en/download/age-of-child-bearing-potential-for-ontario-women-in-2016/
- Bhella S, Gerard L, Lin Y, Rizoli S, Callum J., Obstetric and trauma database review at a single institution finds the optimal maternal age restriction for the transfusion of O- blood to women involved in trauma to be 45 years. Transfusion 2012;52:2488-9.
- Chapman JF. Unlocking the essentials of effective blood inventory management. Transfusion 2007;47:190S-196S.
- Evers D, Middelburg R, deHass M, et al. Red blood cell alloimmunization in relation to antigens’ exposure and their immunogenicity; a cohort study. Lancet, 2016 Jun;3:e284-292.
- Managing Blood and Blood Product Inventory – Guidelines for Australian Health Provinces. April 2013. National Blood Authority, Australia. www.blood.gov.au
- Maternal Age at Delivery Ontario LHINs Five Years of Data; http://transfusionontario.org/en/download/maternal-age-at-delivery-ontario-lhins-five-years-of-data/
- National Advisory Committee on Blood and Blood Products. National Plan for the Management of Shortages of Labile Blood Components; January 18, 2012. http://www.nacblood.ca
- Ontario Regional Blood Coordinating Network. Inventory Management Toolkit; October 30, 2012. http://www.transfusionontario.org
- Stanger SHW et al. Blood inventory management: hospital best practice. Transfus Med Rev, 2012 Apr;26(2):153-63.
Suggested Reading
- Callum JL et al. Bloody Easy 4 Blood Transfusions, Blood Alternatives and Transfusion Reactions. A guide to transfusion medicine. 4th edition. ORBCoN 2016.
- Champion M. Delicate balance; hospital blood inventory management. AABB News, March/April 2004, 34-5.
- Circular of Information for the Use of Human Blood and Blood Components, Canadian Blood Services. www.blood.ca/hospitals
