Chapter 5
Concentrates for hemostatic disorders and hereditary angioedema
NOTE: The product list reflects availability at the time of publication; however, the list is subject to revision on a regular basis and may be revised if changes are required. The product list is regularly updated on blood.ca in the Plasma Protein & Related Products Customer Table of Information (under the section on PPRP dosage, manufacturer and customer information).
Background: Plasma-derived versus recombinant concentrates
This chapter provides detailed information about concentrates for treatment of hemostatic disorders and hereditary angioedema in Canada. Clotting factor concentrates are highly effective treatments for patients with hemostatic disorders caused by missing or defective clotting factors. Clotting factor concentrates may be extracted from pooled donated plasma (plasma-derived) or manufactured using biotechnology (recombinant). Several protein concentrates are available for the treatment of thrombotic disorders and hereditary angioedema.
The factor concentrates available to Canadian patients, as either Health Canada-licensed or unlicensed products, are listed in Table 1a. Access to the unlicensed products and some licensed products that have not undergone Health Canada batch release can be obtained under the Health Canada Special Access Program (SAP) (see note in Table 1a). In addition, a bispecific monoclonal antibody, called emicizumab, that mimics the function of FVIII is now available in Canada. Emicizumab is indicated for hemophilia A patients (congenital factor VIII deficiency) with or without inhibitory antibodies against factor VIII as routine prophylaxis to prevent bleeding or reduce the frequency of bleeding episodes (Table 1b).
Plasma-derived (pd)
The majority of clotting factor concentrates are manufactured from pooled donor plasma.
Recombinant (r)
Recombinant clotting factor concentrates are manufactured using biotechnology. Recombinant products are expressed in cultured cell lines transfected with vectors carrying the clotting factor gene. The recombinant proteins secreted into the culture medium are purified and formulated for therapeutic use. Tables 2 and 3 provide information about the cell lines and the human/animal proteins used during the recombinant product manufacturing process or in the formulation, and the associated allergy precaution required for each recombinant product.
Clotting factor concentrates available in Canada
Factor concentrates available in Canada are listed in Table 1a. Table 1a is based on information available at the time of publication; however, this information is time-sensitive and will change regularly. Please refer to Canadian Blood Services’ Plasma Protein & Related Products Customer Table of Information (under the section on PPRP dosage, manufacturer and customer information) for the most recent updates. Note that some products may be licensed by Health Canada but not carried on the Canadian Blood Services and/or Héma-Québec formulary.
Pharmacokinetic data (IVR, t1/2) may be rounded or generalised; consult product monograph for product-specific information.
Table 1a: Concentrates for hemostasis or hereditary angioedema
| Note: Some products may be licensed by Health Canada but not carried on the Canadian Blood Services and/or Héma-Québec formulary. CBS = carried by Canadian Blood Services, HQ = carried by Héma-Québec, NA = not available; licensed in Canada but not distributed by Canadian Blood Services or Héma-Québec, SAP = currently unlicensed but in use in Canada through the Health Canada Special Access Program. | |||||||||
| No. | Factor concentrate | Manufacturer | Specific viral inactivation/partitioning procedure* | Maximum specific activity ((IU/mg protein) | Storage temp. (oC)/max RT(oC) x (months of RT storage)‡ | Average in vivo recovery (IVR) (IU/dL per IU/kg infused) | Average t1/2 (h) | Assay¥ (for selected products) | Comments |
|---|---|---|---|---|---|---|---|---|---|
| Factor VIII recombinant (rFVIII), human –standard half-life | |||||||||
| 1 | Kovaltry CBS | Bayer Inc. | Solvent detergent/nanofiltration | ~4,000 | 2–8/25 (12) | 2 | 13.8 | Standard aPTT based clotting assay | Full length rFVIII, no VWF |
| 2 | Xyntha® CBS | Pfizer Canada Inc. | Solvent detergent/nanofiltration | 5,500–9,900 | 2–8/25 (3) | 2.11 | 14.8 | Standard aPTT based clotting assay | B-domain deleted FVIII, no VWF |
| 3 | Advate NA | Takeda | Solvent detergent | 4,000-10,000 | 2–8/30 (6) | 2.40 | 11.98 | Standard aPTT based clotting assay | Full length FVIII, no VWF |
| 4 | Nuwiq® HQ | Octapharma | Solvent detergent/nanofiltration | 8,124 | 2–8/25 (1) | 2.14 |
17.1 (age ≥12y) 12.5 (age <12y) |
Standard aPTT based clotting assay | B-domain deleted, no VWF |
| 5 | Zonovate® CBS HQ | Novo Nordisk | Solvent detergent/nanofiltration | 8,300 | 2–8/30 (12) |
1.9 (age ≥12y) 2.0 (age 6–11y) 1.8 (age <6y) |
10.69 (age ≥12y) 8.92 (age 6–11y) 7.65 (age <6y) |
Standard aPTT based clotting assay | B-domain deleted, no VWF |
| Factor VIII, plasma-derived (pd FVIII) – standard half-life | |||||||||
| 6 | Koate®-DVISAP | Grifols | Solvent detergent/terminal dry heat | 9-22 | 2–8/25 (6) | 2.0 | 16.12 | Standard aPTT based clotting assay | pd full length FVIII, contains VWF (VWF:FVIII ratio 1.17:1), formulated with albumin |
| Factor VIII recombinant – extended half-life | |||||||||
| 7 | Adynovate® CBS | Takeda | Solvent detergent | Data not available | 2–8/30 (3) |
2.66 (age ≥ 18y) 2.12 (age 12–17y) |
14.69 (age ≥ 18y) 13.43 (age 12–17y) |
chromogenic or one-stage (no reagent preference) | Recombinant FVIII conjugate with 20 kDa polyethylene glycol (PEGylated rFVIII), no VWF |
| 8 | JiviTM CBS | Bayer Inc. | Solvent detergent/nanofiltration | ~10,000 |
2–8/25 (6) /30 (3) |
Chromogenic: 2.623 One-stage: 2.830 |
~17.6h (age ≥12 y) | chromogenic or one-stage (preference reagents: SynthASil® [Instrumentation Lab]; Pathrombin® [Siemens]) |
B-domain deleted rFVIII conjugated with 60 kDa polyethlene glycol. (PEGylated rFVIII), no VWF |
| 9 | Eloctate® CBS | Bioverativ/ Sanofi | Solvent detergent/nanofiltration | 4,000-10,000 | 2–8/30 (6) | 2.24 | 19 | Standard aPTT based clotting assay | Recombinant fusion protein (B-domain deleted FVIII and dimeric Fc component of human IgG1), no VWF |
| 10 | Esperoct® CBS | Novo Nordisk | nanofiltration | ~10,000 |
2-8/24 (6) 2-8/30 (3) |
Chromogenic: 2.3 |
19.9 (age ≥18y) 15.8 (age 12-<18y) 14.2 (age 6-<12y) 13.6 (age <6y) |
chromogenic, or one-stage (avoid silica-based aPTT reagents - some silica-based aPTT reagents can underestimate FVIII level by up to 50%) |
B-domain truncated (21 aa remaining) rFVIII conjugated with 40 kDa polyethylene glycol (PEGylated rFVIII), no VWF |
| Factor VIII/VWF plasma-derived concentrate (pd FVIII/VWF) (licensed for von Willebrand disease and hemophilia A) | |||||||||
| 11 | Humate-P® CBS HQ | CSL Behring | Pasteurization |
FVIII: 1.3–2.6 VWF:RCo: 3.3–6.6 |
2–25 |
FVIII: 2.0 VWF:RCo: 2.4 |
FVIII: 12.2 VWF:RCo: 11 |
VWF activity/ antigen; FVIII by standard aPTT based clotting assay | VWF: FVIII ratio 2.4:1 |
| 12 | Wilate® CBS | Octapharma | Solvent detergent/terminal dry heat |
≥ 60 IU VWF:RCo ≥ 60 IU FVIII |
2–8/25 (6) | FVIII: 2.04 | FVIII: 15 | VWF activity/ antigen; FVIII by standard aPTT based clotting assay | VWF: FVIII ratio 1:1 |
| Von Willebrand factor concentrate, recombinant (rVWF) | |||||||||
| 13 | Vonvendi® NA | Takeda | Solvent detergent | 110-150 VWF:RCo | 2–30 | 1.5 | 19.1–22.6 | VWF activity/ antigen; FVIII by standard aPTT based clotting assay |
Recombinant VWF, no FVIII 0.7-1.4 IU VWF:RCo/IU VWF:Ag |
| Porcine recombinant FVIII (rpFVIII) | |||||||||
| 14 | Obizur® CBS HQ | Takeda | Solvent detergent/nanofiltration | 11,000–18,000 | 2–8 | PK not yet performed (for acquired hemophilia A) | PK not yet performed (for acquired hemophilia A) | Standard aPTT based clotting assay |
Recombinant Porcine FVIII, no VWF |
| Factor IX recombinant (rFIX) – standard half-life | |||||||||
| 15 | BeneFIX® CBS | Pfizer Canada Inc. | Nanofiltration | ≥ 200 | 2–8/25 (6) |
0.8 (age > 15y); 0.7 (age £ 15y) |
18.8 | Standard aPTT based clotting assay | |
| 16 | Rixubis® HQ | Takeda | Solvent detergent/nanofiltration | ≥ 200 | 2–30 | 0.67 | 26.7 | Standard aPTT based clotting assay | |
| Factor IX high purity plasma derived (pd) – standard half-life | |||||||||
| 17 | Immunine® VH(hep) CBS HQ | Takeda | Vapour heating | 100 ± 50 | 2–8/25 (3) |
1.11 (age > 15y); 0.91 (age £ 15y) |
17 | Standard aPTT based clotting assay |
Contains trace amount of heparin |
| Factor IX recombinant – extended half-life | |||||||||
| 18 |
Alprolix®CBS |
Bioverativ | Nanofiltration |
45–63 |
2–8/30 (6) |
0.92 | 82.1 | Standard aPTT based clotting assay |
Recombinant fusion protein of FIX and dimeric Fc component of human IgG1 (rFIXFc) |
| 19 | REBINYN® CBS | Novo Nordisk | Nanofiltration | 152 | 2–8/30 (6) |
1.9 (age ≥ 18y age) 1.8 (age 13–17y age) |
115 (age ≥ 18y) 103 (age 13–17y) |
chromogenic or one-stage (preferred reagents: SynthAFax®, [Instrumentation Lab]; STA®-Cephascreen [Diagnostica Stago] | Recombinant FIX conjugate with 40 kDa polyethylene glycol (PEGylated rFIX) |
| 20 | Idelvion® NA | CSL-Behring | Solvent/detergent, Nanofiltration | ≥53 | 2–25 |
1.3 (age ≥ 12y) 1.0 (age < 12y) |
104.2 (age ≥ 18y) 87.3 (age 12 to <18y 91.0 (age 1 to <12y) |
one-stage clotting (NOTE: use of kaolin-based aPTT reagent or Actin FS aPTT reagent will likely result in an underestimation of FIX activity) | Recombinant fusion protein of FIX and albumin. |
| Prothrombin Complex Concentrate (pd) (pd PCC) | |||||||||
| 21 | Beriplex® P/N(hep)CBS HQ | CSL Behring | Pasteurization/ nanofiltration | Data not available | 2–25 |
FVII: 2.47 FIX: 1.64 |
FVII: 4 FIX: 17 |
Standard PT/aPTT based clotting assays | Heparin, Proteins C and S added |
| 22 | Octaplex® (hep) CBS | Octapharma | Solvent detergent/ nanofiltration | FIX: ≥ 0.6 | 2–25 |
FVII: 0.84–1.24 FIX: 0.8–1.42 |
FVII: 5.4–8.3 FIX: 28.7–49.1 |
Standard PT/aPTT based clotting assays | Heparin, Proteins C and S added |
| Activated Prothrombin Complex Concentrate (pd) (pd aPCC) | |||||||||
| 23 | FEIBANF CBS HQ | Takeda | Vapour heat/ nanofiltration | 0.75–2.5 | 2–25 | Data not available | 6–12 | Standard PT/aPTT based clotting assays |
No heparin added; FII, FVII, FIX and FX in relatively balanced ratio; 89–98% FVII activity attributed to FVIIa activity |
| Fibrinogen (pd) | |||||||||
| 24 |
RiaSTAP® CBS HQ |
CSL Behring | Pasteurization | 0.68 mg/mg‡ | 2–25 | 0.017 (g/L per mg/kg body weight infused) | 77.1 | Standard clot-based assay | 400–700 mg of human albumin per 1 g concentrate |
| 25 | Fibryga® CBS | Octapharma | Solvent-detergent/ nanofiltration (20 nm) |
98 ± 0.7% (total clottable protein) 1 |
2–25 | 0.018 (g/L per mg/kg body weight infused) | 75.9 | Standard clot-based assay |
500 mg glycine per g concentrate No human albumin added. |
| Factor VII (pd) (pd FVII) | |||||||||
| 26 | Factor VII (hep) SAP | Takeda | Vapour heat/ nanofiltration | ≥ 2 | 2–8 | 1.2–2.0 | 3–5 | Standard PT based clotting assay |
Heparin added |
| Factor VIIa Recombinant (rFVIIa) | |||||||||
| 27 | NiaStase RT® CBS HQ | Novo Nordisk | Detergent | 50,000 | 2–25 | 45.6% / 43.5% (non-bleeding / bleeding state) | 2.9 / 2.3 (non-bleeding / bleeding state) | Standard PT based clotting assay | |
| Factor X (pd) (pd FX) | |||||||||
| 28 | Factor X P Behring(hep) SAP | CSL Behring | Pasteurization |
FX: 4-60 FIX: 3-38 |
2–8/24 |
FX: 1-2 FIX: 1.08 (SD 0.30) |
FX: 24-40h FIX: 22h |
Standard PT based clotting assay | No FII and FVII, Heparin, AT added |
| Factor XI (pd) (pd FXI) | |||||||||
| 29 | Factor XI(hep) SAP | Bio Products Laboratory (UK) | High dry heat | 35 | 2–8 or 2–25 (depending on lot number) | 2.4 | 48 | Standard aPTT based clotting assay | Heparin, AT added |
| Factor XIII Recombinant (rFXIII) | |||||||||
| 30 | Tretten® CBS | Novo Nordisk | Not applicable | 116–223 | 2–8 | 1.7 | (11.5d) | Clot solubility assay for severe deficiency screening. Specialized assays (e.g. Chromogenic) for FXIII activity level
Contains FXIII-A subunit only, not recommended for FXIII-B subunit deficiency |
Contains FXIII-A subunit only, not recommended for FXIII-B subunit deficiency |
| Factor XIII (pd) (pd FXIII) | |||||||||
| 31 |
Corifact®CBS HQ |
CSL Behring | Pasteurization/ nanofiltration | 5.7–8.9 | 2–8 | 1.66 | (6.6d) |
Clot solubility assay for severe deficiency screening. Specialized assays (e.g., Chromogenic) for FXIII activity level. |
Contains both FXIII-A and FXIII-B subunits |
| Antithrombin (pd) | |||||||||
| 32 | Antithrombin III NF®(hep) CBS HQ | Takeda | Vapor heat, nanofiltration | 1–2.5 | 2–8 | ~2 | (2.5d) | Specialized assays for antithrombin activity/antigen levels | Heparin added |
| Protein C (pd) | |||||||||
| 33 | CeprotinSAP | Takeda | Pasteurization/ detergent | Data not available | 2–8 | 1.42 | 9.9 | Specialized assays for protein C activity/antigen levels | Human albumin added |
| C1-Inhibitor (pd) for Hereditary Angioedema (HAE) | |||||||||
| 34 | Berinert® CBS HQ | CSL Behring |
Pasteurization, nanofiltration |
Data not available | 2–30 | Data not available | 87.7–91.4 | Specialized assays for C1-inhibitor activity/antigen levels | |
| 35 | CINRYZE® CBS | Takeda | Pasteurization, nanofiltration | 4.0–9.0 IU/mg protein | 2–25 | Data not available | 56 | Specialized assays for C1-inhibitor activity/antigen levels | |
| 36 | HAEGARDATM CBS HQ | CSL-Behring | Pasteurization, nanofiltration | Data not available | 2–30 | Data not available | Median (2.9d/69h) (95%CI 1d, 10.4d) | Specialized assays for C1-inhibitor activity/antigen levels | For subcutaneous injections for prophylaxis (not approved for acute treatment) |
|
Abbreviations: IVR=in vivo recovery; pd=plasma-derived; r=recombinant; RCo=Ristocetin cofactor; RT=room temperature; VWF=von Willebrand factor; t ½=half-life; h=hour(s); d=day(s); y=year(s)
* Specific viral inactivation/partitioning procedure completed in addition to chromatographic fractionation/purification steps routinely used in the manufacturing process that can remove virus particles. ‡Maximum room temperature (RT) (usually ≤25°C or ≤30°C) storage period in months is stated only if the concentrate is to be stored refrigerated (2–8°C). Manufacturers recommend that once the concentrate has been removed from the required refrigeration and stored at RT, the date removed from refrigeration should be marked on the box and the product should not be returned to refrigeration. ¥ Assay: for clotting factor concentrates, unless otherwise stated in the Comments section, one-stage clotting assays are adequate as generally used in Canada. For certain glyco-PEGylated products, one-stage assays are best performed with the indicated preferred reagents; otherwise, chromogenic assays should be used. (hep) Contains heparin – contraindicated in patients with a history of heparin-induced thrombocytopenia. |
|||||||||
Ordering
For licensed products, contact Canadian Blood Services or Héma-Québec.
For all unlicensed and some licensed products not yet batch-released by Health Canada, contact the Health Canada Special Access Program (SAP). Regular business hours are weekdays from 8:30 am to 4:30 pm Eastern Standard Time (EST). Fax all requests to (613) 941-3194. For after hours and urgent requests requiring immediate attention please follow up with a call to the SAP at: (613) 941-2108 (available 24/7).
Notes on factor concentrates
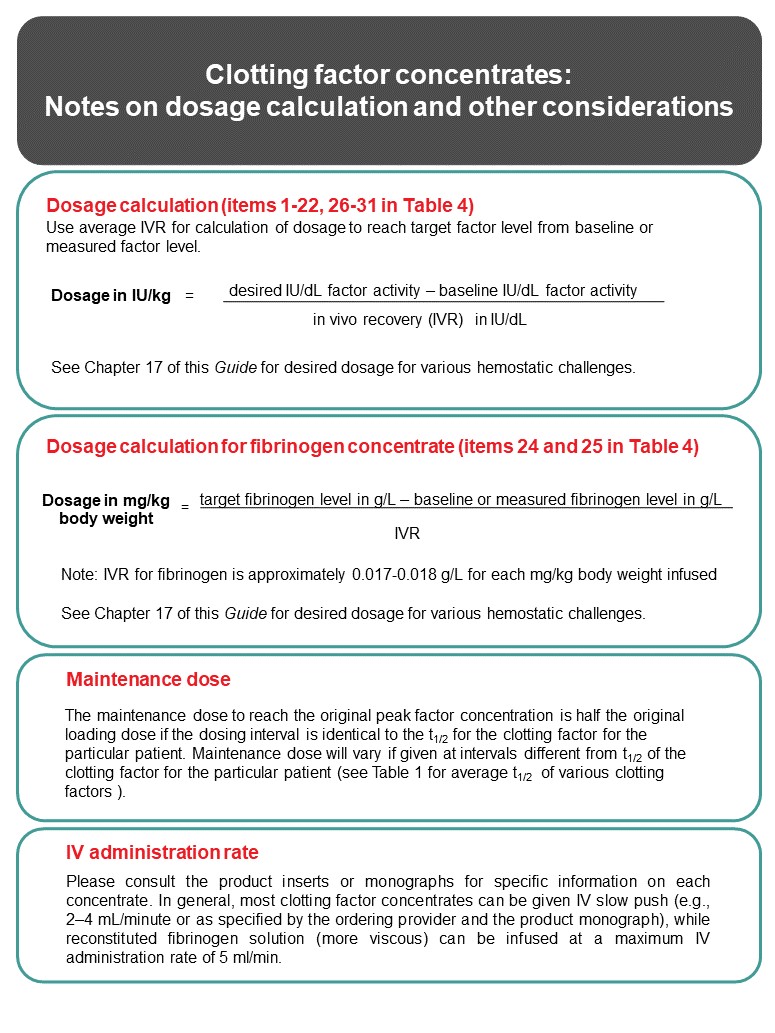
Recovery or IVR (activity in IU/dL recovered in circulation after 1 IU/kg infused) and half-life (t1/2) were established in patients with severe congenital deficiency, not in patients with acquired deficiency. For antithrombin and protein C products, recovery and t1/2 are expected to be lower during acute thrombotic events. See Figure 1 for notes on dosing.
Recovery and t1/2 indicated here are provided as rough guides only—the precise recovery and t1/2 may be different from patient to patient and can be determined by pharmacokinetic studies to help with more precise dosing and dosing intervals (see Chapter 17 of this Guide). Recovery tends to be lower in children, who have higher plasma volumes.
Non-clotting factor product
Emicizumab (Hemlibra®), bispecific monoclonal antibody to FIX/FIXa and FX/FXa is a non-clotting factor product manufactured by recombinant technology.
- produced in Chinese hamster ovary (CHO) cells (allergy precaution: trace hamster proteins)
- human-animal protein present in cell culturing but removed during manufacturing process (allergy precaution: trace bovine proteins)
Current criteria for access to Hemlibra® through Canadian Blood Services is:
- Congenital hemophilia A with inhibitors to factor VIII
- Severe congenital hemophilia A (intrinsic factor VIII level < 1%) without inhibitors
Table 1b: Non-clotting factor product for hemostasis available in Canada
| Note: Some products may be licensed by Health Canada but not carried on the Canadian Blood Services and/or Héma-Québec formulary. CBS = carried by Canadian Blood Services, HQ = carried by Héma-Québec | |||||||||
| No. | Product | Manufacturer | Specific viral inactivation/partitioning procedure* | Product Cmax (µg/mL) | Storage temp. (oC)/max RT(oC) x (days of RT storage) ¥ | Mean trough (µg/mL) | Average t1/2 (d) | Assay for selected products | Comments |
|---|---|---|---|---|---|---|---|---|---|
| 37 | Hemlibra® CBS HQ (emicizumab) | Hoffman-La Roche | Low pH hydrochloric acid/nanofiltration |
55.1±15.9 (dose 1.5 mg/kd QW)
58.3±16.4 (dose 3 mg/kg Q2W)
67.0±17.7 (dose 6 mg/kg Q4W) (administered subcutaneously) |
2-8 (7 d at RT) |
52.6±13.6 (at week 5 following loading dose at 3 mg/kg weekly x 4 weeks) (administered subcutaneously) |
26.9 d | Use chromogenic FVIII assay with bovine reagents for assessment of FVIII activity and FVIII inhibitor titer |
|
|
Abbreviations: Cmax=peak concentration; RT=room temperature; t½=half-life; d=day(s)
*Specific viral inactivation/partitioning procedure completed in addition to chromatography fractionation/purification steps routinely used in the manufacturing process that are capable of removing virus particles. ¥ Maximum room temperature (RT) (usually ≤25°C or ≤30°C) storage period in months is stated only if the concentrate is to be stored refrigerated (2–8°C). Manufacturers recommend that once the concentrate has been removed from the required refrigeration and stored at RT, the date removed from refrigeration should be marked on the box and the product should not be returned to refrigeration. |
|||||||||
Administration
Hemlibra® (emicizumab) is administered subcutaneously for bleeding prophylaxis in hemophilia A patients with or without inhibitors:
- Loading dose: 3 mg/kg weekly x 4 weeks
- Maintenance dose:
- 1.5 mg/kg weekly, or
- 3 mg/kg biweekly, or
- 6 mg/kg every 4 weeks
Note: the maintenance dose of 6 mg/kg once every 4 weeks is not recommended for patients <40 kg body weight or patients <12 years of age.
Viral safety
The chromatographic process used during fractionation and purification of the clotting factors reduces the viral load.
Additionally, virus inactivation/partitioning procedures are incorporated into the manufacturing process for all plasma derived concentrates and most of the recombinant concentrates (see Tables 1a and 1b).
- The virus inactivation procedures are all effective against important human pathogens such as human immunodeficiency virus (HIV), hepatitis C virus (HCV) and hepatitis B virus (HBV). In Canada, virus-inactivated factor concentrates were introduced in 1985. No case of HIV or HCV transmission due to concentrate use has occurred since 1987 and 1988, respectively.
- However, no virus inactivation procedure is expected to inactivate all viruses. In particular, non-enveloped viruses such as parvovirus B19, a pathogen in immunosuppressed patients, can be resistant to viral inactivation processes.
Patients with congenital coagulation deficiency who are expected to receive any blood product(s) should be immunized against HBV and hepatitis A virus (HAV).
Transmission of Creutzfeld-Jakob disease (CJD) and variant CJD is considered a theoretical risk for plasma derived concentrates.
Prevention of thrombotic complications
Clotting factor concentrates affect hemostasis by correcting the underlying clotting defect.
Patients with clotting factor deficiency and with coexisting risk factors for thrombosis or disseminated intravascular coagulation (DIC) may develop thrombotic complications when the hemostatic mechanism is corrected.
Factor eight inhibitor bypass activity (FEIBA), factor XI (FXI) concentrate and recombinant factor VIIa (rFVIIa) should be used with caution and under the guidance of a hematologist/thrombosis or transfusion specialist physician in patients with risk factors for thrombosis or DIC.
Prothrombin complex concentrate (PCC) and activated prothrombin complex concentrate (aPCC) should be administered as directed on the package insert to prevent thrombotic complications. It is not indicated for liver disease, DIC, or patients with active arterial or venous thromboembolism or with underlying thrombotic risks. Use of PCC and aPCC has been reported to result in myocardial infarction and intracardiac thrombus.1-3 Due to presence of heparin, it is contraindicated in those with a history of heparin-induced thrombocytopenia (HIT).
The dosage for FEIBA should not exceed 200 IU/kg/day.
- Patients on Hemlibra® (emicizumab) prophylaxis
- should avoid using aPCC or PCC because of the risk of thromboembolism and thrombotic microangiopathy (TMA).
- If aPCC must be used, the dose should NOT exceed 50 IU/kg/dose or 100 IU/kg/day with TMA monitoring
- Hemlibra® has a half-life of ~4 weeks and remains in circulations for months after discontinuation. aPCC and PCC should not be used for 6 months after Hemlibra® has been stopped
- The dosage for FXI concentrate should not exceed 30 IU/kg per dose.
- Thrombosis has been reported in patients with von Willebrand disease (VWD), treated to raise factor VIII (FVIII) level in excess of 200 IU/dL (2 IU/ml) in the surgical setting.
- Antifibrinolytic therapy should be avoided when using PCC and aPCC (including FEIBA).
Several plasma-derived concentrates contain heparin (Factor VII concentrate [Takeda], FX®P [CSL-Behring], FXI Factor XI concentrate [BPL], FIX Immunine® VH [Takeda], PCC Beriplex® P/N [CSL Behring], PCC Octaplex® [Octapharma], Antithrombin III NF [Takeda]; see Table 1a). These concentrates should be avoided in patients with a history of heparin-induced thrombocytopenia.
Allergy precautions
As with infusion of any protein products, allergic reactions may occur.
- Minor allergic reactions may be prevented by pre-medication with antihistamines.
- When an allergic reaction occurs, a similar concentrate from a different manufacturer can be used for subsequent treatment and may not result in an allergic response.
- Patients on home-therapy should have epinephrine (e.g., Epipen®) on hand to deal with serious allergic reactions or anaphylaxis.
- Some recombinant concentrates or products may contain trace amount of non-human proteins (see Tables 2 and 3). The manufacturers suggest caution in the use of their respective products in patients with known allergy to these proteins. Recombinant porcine FVIII is of porcine protein in nature.
Hemophilia B patients may have severe allergic responses (including anaphylaxis) to concentrates containing factor IX (FIX) (including prothrombin complex concentrates and FEIBA) at the time inhibitors are developing.
- In susceptible severe hemophilia B patients, inhibitors develop usually early on with FIX concentrate treatment.
- It is advisable to treat newly diagnosed severe hemophilia B patients in a setting equipped for management of severe allergic reactions during at least the initial 10-20 treatments.4
Table 2: Cell lines used for the manufacturing of various recombinant factor concentrate
| Cell lines | Recombinant concentrates | Allergy precaution |
|---|---|---|
| Baby hamster kidney (BHK) |
rFVIII - KovaltryTM (Bayer) rFVIII - JiviTM (Bayer) rFVIII porcine - Obizur® (Takeda) rFVIIa - Niastase RT® (Novo Nordisk) |
Trace hamster proteins |
| Chinese hamster ovary (CHO) |
rFVIII - Advate (Shire) - Adynovate® (Takeda) - Esperoct® (Novo Nordisk) - Xyntha® (Pfizer) - Zonovate® (Novo Nordisk) rFIX - BeneFIX® (Pfizer) - Rixubis® (Takeda) - Rebinyn® (Novo Nordisk) - Idelvion® (CSL-Behring) rVWF - Vonvendi® (Takeda) |
Trace hamster proteins |
| Human embryonic kidney (HEK) |
rFVIII - Nuwiq® (Octapharma) rFVIIIFc - Eloctate® (Bioverativ/Sanofi) rFIXFc - Alprolix® (Bioverativ/Sanofi) |
|
| Yeast (Saccharomyces cerevisiae) | rFXIII - Tretten® (Novo Nordisk) | Trace yeast proteins |
Table 3: Human/animal proteins that may be present during the manufacturing process (cell culturing or purification) or in formulation in recombinant factor concentrates
| Proteins | Recombinant concentrates | Allergy precaution |
|---|---|---|
| Solid phase mouse monoclonal antibody – for purification step |
rFVIII - Advate® (Takeda) - Adynovate® (Takeda) - Esperoct® (Novo Nordisk) - KovaltryTM (Bayer) - JiviTM (Bayer) - Zonovate® (Novo Nordisk) |
Trace mouse proteins |
| Concentrate of porcine protein | Porcine rFVIII – Obizur® (Takeda) | Porcine protein |
| Human serum albumin in formulation | Human serum albumin no longer used in recombinant products currently available in Canada |
Storage and transportation
Clotting factor concentrates are stable until the printed expiration date on the vials (or boxes) when stored at the specified temperature.
- For products that are to be refrigerated at 2–8°C (see Tables 1a, 1b), long distance transportation must occur in validated transport containers cooled with cold packs.
- Some, but not all, of these concentrates can be stored at RT (usually ≤25°C or ≤ 30°C) for a specified period after removing from the refrigerated temperature (see Table 1).
- When it is necessary to store these products at RT, the date when the box is removed from refrigeration must be clearly marked on the box, and the manufacturers do not recommend returning these RT stored concentrates to refrigeration.
- Storage of concentrates at freezing temperature should be avoided.
Reconstitution
Almost all clotting factor concentrates available to Canadian patients are supplied in packages containing a kit for reconstitution and infusion, usually with the appropriate diluent.
Many manufacturers also provide proprietary devices for transferring diluent into the vial containing the lyophilized concentrate and for withdrawing the dissolved concentrate to syringes for infusion. The reconstitution instructions in the product insert must be followed and aseptic techniques observed.
In general, the vials of diluent and concentrate should be at room temperature (or pre-warmed to 20–37oC for refrigerated products) before mixing. The diluent should, if possible, be allowed to flow down the side of the vial wall and the mixture should then be swirled gently to allow dissolution of the concentrate. Shaking must be avoided as it may create bubbles/foam and result in denaturation of the proteins.
Specific properties and indications of factor concentrates
Table 4 below provides indications, monitoring, contraindications/precautions and available alternatives for different classes of factor concentrates (Table 1a) and nonfactor product (Table 1b). For specific product information refer to the package insert provided by the manufacturer of each concentrate.
Table 4: Use of clotting factor concentrates and nonfactor product
| Item No. (refer to Tables 1a/1b) | Factor concentrate | Indications (for treatment and prophylaxis)* | Monitoring | Contraindications/precautions | Available alternatives |
|---|---|---|---|---|---|
| 1-5 | rFVIII (standard half-life) |
|
|
|
|
| 6-7 | High purity pdFVIII (standard half-life) |
|
|
|
|
| 8-10 | rFVIII (extended half-life) |
|
|
|
|
| 11-12 | pd FVIII/VWF |
|
|
|
|
| 13 | rVWF |
|
|
|
|
| 14 | rPorcine FVIII |
|
|
|
|
| 15-16 | rFIX (standard half-life) |
|
|
|
|
| 17 | High purity pd FIX (standard half-life) |
|
|
|
|
| 18-20 | rFIX (extended half-life) |
|
|
|
|
| 21-22 | pd PCC, non-activated (contains FII, FVII, FIX, FX) |
|
|
|
|
| 23 | pd aPCC |
|
|
|
|
| 24-25 | pd Fibrinogen |
|
|
|
|
| 26 | pd FVII |
|
|
|
|
| 27 | rFVIIa |
|
|
|
|
| 28 | pd FX/FIX |
|
|
|
|
| 29 |
pd FXI |
|
|
|
|
| 30 | rFXIII |
|
|
|
|
| 31 | pd FXIII |
|
|
|
|
| 32 | pd antithrombin |
|
|
|
|
| 33 | pd protein C |
|
|
|
|
| 34-36 | pd C1-INH |
|
|
|
|
| 37 | Hemlibra® |
|
|
|
|
|
Abbreviations: aPCC = activated Prothrombin Complex Concentrate; AT = antithrombin; FEIBA = Factor eight inhibitor bypass activity; INR = International Normalized Ratio; ITI = Immune Tolerance Induction; PCC = prothrombin complex concentrate; pd = plasma derived; RCo = Ristocetin Cofactor; VWD = von Willebrand disease; VWF = von Willebrand Factor; * Plasma: Virus inactivated plasma such as Octaplasma® (Octapharma) preferred over fresh frozen plasma or frozen plasma ‡ see National Advisory Committee and Blood and Blood Products (NAC) 2022 recommendations for use of Prothrombin Complex Concentrates ⁋ PCC and fibrinogen for acquired bleeding disorders: please see next section on “Additional information on use of selected concentrates.” |
|||||
Additional information on use of selected concentrates
Prothrombin complex concentrates for acquired bleeding disorders (Table 4, items 21-22)
- For rapid reversal of warfarin anticoagulant (or severe Vitamin K deficiency) in patients with severe bleeding or requiring emergency surgery (see also Chapter 17 of this Guide): for dosage at different INR, please consult National Advisory Committee on Blood and Blood Products (NAC) 2022 recommendations on use of prothrombin complex concentrates, as well as the Thrombosis Canada clinical guides.
- For reversal of DOAC (anti-Xa) in patients with severe bleeding or requiring emergency surgery (see also Chapter 17 of this Guide) and when specific antidote (Andexanet alfa [AndexXa®]) is not available. Dosage: 25-50 IU/kg, maximum 3000 IU
For treatment of dilutional coagulopathy with acquired clotting factors deficiency. A Canadian pilot study suggested 4-factor PCC may be a suitable alternative to fresh plasma for management of bleeding following cardiac surgery.5
Activated prothrombin complex concentrate for acquired bleeding disorders (Table 4, item 23)
- For reversal of DOAC (anti-IIa, Dabigatran®) in patients with severe bleeding or requiring emergency surgery (see also Chapter 17 of this Guide) and when specific antidote (idarucizumab [Praxbind®) is not available. Dosage 50 IU/kg, maximum 2000 IU. For more information, please consult the Thrombosis Canada clinical guides and the 2022 NAC recommendations on use of prothrombin complex concentrates.
Fibrinogen concentrates for acquired fibrinogen deficiency (Table 4, items 24-25)
Fibrinogen concentrates are safe and effective alternatives to cryoprecipitates and plasma in severe bleeding with hypofibrinogenemia following surgery/trauma and in association with dilutional and consumptive coagulopathies (e.g., massive transfusion, see Chapter 11 of this Guide).6 The Canadian FIBRES randomized clinical trial showed that 4 g fibrinogen concentrate was non-inferior to 10 units cryoprecipitates for patients with significant bleeding and hypofibrinogenemia following cardiac bypass surgery.7
Antithrombin concentrate for congenital antithrombin deficiency (Table 4, item 32)
Antithrombin concentrate together with heparin has been used in patients with inherited antithrombin deficiency and heparin resistance, as prophylaxis for surgery, trauma, immobilization, and thromboembolism during pregnancy as well as after delivery, with favourable results.8 There are, however, no randomized clinical trials to establish efficacy. One recommendation for dosage calculation is as follows: Loading dose: [(target minus current AT level in IU/dL) x weight (kg) ¸ 1.4]; maintenance dose: ~60% loading dose every 24h to maintain peak AT level at ~120 IU/dL and trough level at ~80 IU/dL.
Protein C concentrate (item 33 in Table 4) for congenital protein C deficiency.9
Patients with homozygous or compound heterozygous protein C deficiency typically present with skin necrosis within the first two weeks of postnatal life. Replacement therapy with protein C concentrate at a dose of 100 IU/kg followed by 50 IU/kg every 6 hours to maintain a trough protein C level of about 50 IU/dL (as well as decreasing or normalization of D-dimer level) can be used.
For long-term prophylaxis in patients with severe protein C deficiency (homozygous/compound heterozygous), maintenance subcutaneous (or intravenous) doses of 30–50 IU/kg every one to two days or warfarin (initiated after full heparinization for several days to prevent skin necrosis) to maintain INR 2.5–3.5 (or INR 1.5–2.5 together with protein C replacement) have been used. Monitoring with D-dimer level for evidence of coagulation activation is useful to confirm adequate replacement or anticoagulation therapy.
Hemlibra® or emicizumab (item 37 in Table 4) for prophylaxis in hemophilia A patients with or without FVIII inhibitors
A monoclonal bispecific antibody binding both FIXa/FIX and FX/FXa mimicking the cofactor function of FVIII to activate FX to FXa, is used for prophylaxis of hemophilia A with or without inhibitor antibodies to FVIII.10 For loading dose and maintenance doses, please see the section on non-clotting factor product and Table 1b. In patient using Hemlibra®, avoid concomitant use of aPCC (FEIBA) which may result in thromboembolism and thrombotic microangiopathy (see section on “Prevention of Thrombotic Complications”). Hemlibra® interferes with aPTT-based clotting assays, artificially shortening aPTT and increasing FVIII activity. Chromogenic assay using bovine reagents should be used for FVIII and FVIII inhibitor assessment. It does not affect PT-based clotting factor assays or thrombin time.11
Further reading and sources
The product monographs/package inserts should be consulted for further information about the various products discussed in this chapter. See Chapter 17 of this Guide for more information on hemostatic disorders.
The information presented in this chapter was obtained from the individual manufacturers, usually vetted through their medical/scientific and regulatory departments, and from product monographs available online. Where possible, data from different sources were compared to each other and to the literature. It should be noted that parameters such as average IVR and t1/2 are approximate and may differ slightly from different sources including those from different studies and different phases of clinical trials.
Continuing professional development credits
Fellows and health-care professionals who participate in the Canadian Royal College's Maintenance of Certification (MOC) program can claim the reading of the Clinical Guide to Transfusion as a continuing professional development (CPD) activity under Section 2: Individual learning. Learners can claim 0.5 credits per hour of reading to a maximum of 30 credits per year.
Medical laboratory technologists who participate in the Canadian Society for Medical Laboratory Science’s Professional Enhancement Program (PEP) can claim the reading of the Clinical Guide to Transfusion as a non-verified activity.
Acknowledgements
The authors acknowledge Kathryn Webert, MD, MSc, FRCPC; Aditi Khandelwal, MDCM, FRCPC; and Caitlin Jones, BScPhm, RPh, PharmD, MScHQ, for their review of this chapter.
Suggested citation
Poon M, Goodyear D, Rydz N, Lee A. Concentrates for hemostatic disorders and hereditary angioedema. In: Clarke G, Abe T, editors. Clinical Guide to Transfusion [Internet]. Ottawa: Canadian Blood Services, 2022 [cited YYYY MM DD]. Chapter 5. Available from: https://professionaleducation.blood.ca
If you have questions about the Clinical Guide to Transfusion or suggestions for improvement, please contact us through the Feedback form.
References
- Warren O, Simon B. Massive, Fatal, Intracardiac Thrombosis Associated with Prothrombin Complex Concentrate. Annals of Emergency Medicine 2009; 53: 758-61. https://doi.org/10.1016/j.annemergmed.2008.12.027.
- Goldhammer JE, Bakowitz MJ, Milas BL, Patel PA. Intracardiac Thrombosis after Emergent Prothrombin Complex Concentrate Administration for Warfarin Reversal. Anesthesiology 2015; 123: 458-458. https://doi.org/10.1097/ALN.0000000000000464.
- Mar PL, Brown LE, Chong L, Gopinathannair R. Multichamber Intracardiac Thrombosis During Novel Oral Anticoagulation Reversal with Activated Prothrombin Complex Concentrate Infusion. HeartRhythm Case Reports 2020; 6: 144-7. https://doi.org/10.1016/j.hrcr.2019.11.010.
- Srivastava A, Santagostino E, Dougall A, Kitchen S, Sutherland M, Pipe SW, Carcao M, Mahlangu J, Ragni MV, Windyga J, Llinás A, Goddard NJ, Mohan R, Poonnoose PM, Feldman BM, Lewis SZ, van den Berg HM, Pierce GF, on behalf of the WFH Guidelines for the Management of Hemophilia panelists and co-authors. WFH Guidelines for the Management of Hemophilia, 3rd Edition. Haemophilia 2020; 26: 1-158. https://onlinelibrary.wiley.com/doi/abs/10.1111/hae.14046.
- Karkouti K, Bartoszko J, Grewal D, Bingley C, Armali C, Carroll J, Hucke H-P, Kron A, McCluskey SA, Rao V, Callum J. Comparison of 4-Factor Prothrombin Complex Concentrate with Frozen Plasma for Management of Hemorrhage During and after Cardiac Surgery: A Randomized Pilot Trial. JAMA Network Open 2021; 4: e213936-e. https://doi.org/10.1001/jamanetworkopen.2021.3936.
- Franchini M, Lippi G. Fibrinogen Replacement Therapy: A Critical Review of the Literature. Blood Transfus 2012; 10: 23-7. https://pubmed.ncbi.nlm.nih.gov/22153684
- Callum J, Farkouh ME, Scales DC, Heddle NM, Crowther M, Rao V, Hucke H-P, Carroll J, Grewal D, Brar S, Bussières J, Grocott H, Harle C, Pavenski K, Rochon A, Saha T, Shepherd L, Syed S, Tran D, Wong D, Zeller M, Karkouti K, Group ftFR. Effect of Fibrinogen Concentrate Vs Cryoprecipitate on Blood Component Transfusion after Cardiac Surgery: The Fibres Randomized Clinical Trial. JAMA 2019; 322: 1966-76. https://doi.org/10.1001/jama.2019.17312.
- Patnaik MM, Moll S. Inherited Antithrombin Deficiency: A Review. Haemophilia 2008; 14: 1229-39. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2516.2008.01830.x.
- Goldenberg NA, Manco-Johnson MJ. Protein C Deficiency. Haemophilia 2008; 14: 1214-21. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2516.2008.01838.x.
- National Hemophilia Foundation. Masac Document 258 - Recommendation on the Use and Management of Emicizumab-Kxwh (Hemlibra®) for Hemophilia a with and without Inhibitors. National Hemophilia Foundation, 2020. https://www.hemophilia.org/healthcare-professionals/guidelines-on-care/masac-documents/masac-document-258-recommendation-on-the-use-and-management-of-emicizumab-kxwh-hemlibrar-for-hemophilia-a-with-and-without-inhibitors.
- Nogami K, Shima M. New Therapies Using Nonfactor Products for Patients with Hemophilia and Inhibitors. Blood 2019; 133: 399-406. https://doi.org/10.1182/blood-2018-07-820712.